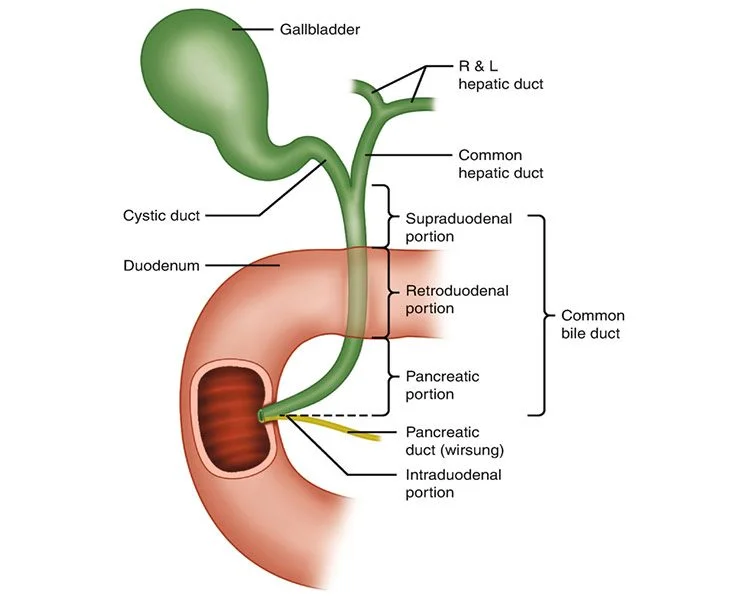
Patients with severe insulin resistance (SIR) often present with complex metabolic and gastrointestinal complications, including biliary tract disorders. The intricate relationship between insulin resistance, bile acid metabolism, and hepatic function necessitates a targeted approach to diagnosis. This article outlines the optimal diagnostic strategies for identifying biliary tract abnormalities in patients with SIR, emphasizing advanced imaging modalities and laboratory assessments.
Pathophysiology of Biliary Tract Disorders in Severe Insulin Resistance
Insulin resistance disrupts normal bile composition and flow, predisposing individuals to gallstones, biliary dyskinesia, and cholestasis. Key mechanisms include:
- Impaired Bile Acid Homeostasis: Dysregulated bile acid synthesis and secretion lead to lithogenic bile, increasing gallstone risk.
- Hepatic Steatosis and Inflammation: Insulin-resistant states promote nonalcoholic fatty liver disease (NAFLD), which can exacerbate biliary dysfunction.
- Dysmotility of the Biliary System: Altered neuromuscular control of the gallbladder and sphincter of Oddi contributes to functional biliary disorders.
These factors necessitate a nuanced diagnostic approach that integrates clinical evaluation, biochemical markers, and advanced imaging.
Clinical Presentation and Red Flags
Patients with severe insulin resistance may exhibit atypical or overlapping symptoms, making diagnosis challenging. Common symptoms include:
- Right upper quadrant pain
- Postprandial nausea and bloating
- Jaundice in advanced cases
- Unexplained fluctuations in liver function tests (LFTs)
- Persistent pruritus (suggesting intrahepatic cholestasis)
Identifying these symptoms early is crucial to prevent complications such as biliary obstruction and secondary infections.
Key Diagnostic Tests and Biomarkers
1. Liver Function Tests (LFTs)
LFTs provide initial biochemical insights into biliary function:
- Elevated Alkaline Phosphatase (ALP) & Gamma-Glutamyl Transferase (GGT): Indicative of cholestasis or bile duct obstruction.
- Bilirubin Levels: Direct hyperbilirubinemia suggests obstructive pathology.
- Aminotransferases (AST & ALT): Markers of hepatocellular injury often seen in concurrent NAFLD.
2. Serum and Urinary Bile Acids
Increased serum bile acids suggest hepatic or biliary dysfunction. Urinary bile acid profiling can help differentiate intrahepatic from extrahepatic cholestasis.
3. Fasting Insulin and HOMA-IR Index
Assessing insulin resistance severity may provide indirect insights into metabolic contributions to biliary dysfunction.
Advanced Imaging Modalities
1. Abdominal Ultrasound (USG)
First-line imaging modality for detecting gallstones, bile duct dilation, and sludge. However, its sensitivity may be reduced in obese patients with severe insulin resistance.
2. Endoscopic Ultrasound (EUS)
Superior sensitivity for microlithiasis and biliary strictures, particularly in patients with inconclusive transabdominal ultrasound findings.
3. Magnetic Resonance Cholangiopancreatography (MRCP)
Non-invasive, high-resolution imaging for detailed bile duct visualization and evaluation of structural abnormalities.
4. Endoscopic Retrograde Cholangiopancreatography (ERCP)
Reserved for therapeutic intervention in cases of confirmed obstruction, strictures, or stone-related complications.
5. Hepatobiliary Iminodiacetic Acid (HIDA) Scan
Functional assessment of gallbladder motility and bile flow, particularly useful for diagnosing biliary dyskinesia in insulin-resistant patients.