Diabetic nephropathy (DN) is a progressive kidney disease caused by long-term diabetes mellitus, characterized by glomerular damage, proteinuria, and eventual renal failure. The presence of severe insulin resistance (SIR) exacerbates DN, accelerating renal deterioration and complicating glycemic control. This article provides an in-depth exploration of DN with SIR, including its pathophysiology, risk factors, diagnosis, and state-of-the-art management approaches.
Pathophysiology of Diabetic Nephropathy with Severe Insulin Resistance
DN develops due to chronic hyperglycemia, which induces metabolic and hemodynamic changes that damage renal structures. Severe insulin resistance, often associated with metabolic syndrome and obesity, further exacerbates this condition.
1. Mechanisms Involved
- Hyperglycemia-Induced Damage: Persistent high blood sugar leads to advanced glycation end-products (AGEs) formation, oxidative stress, and inflammation.
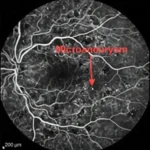
- Glomerular Hypertension: Increased intraglomerular pressure due to impaired endothelial function and renin-angiotensin-aldosterone system (RAAS) activation accelerates nephron loss.
- Podocyte Dysfunction: Insulin plays a role in podocyte survival. Severe insulin resistance results in podocyte injury, leading to proteinuria and glomerular sclerosis.
- Lipotoxicity: Elevated circulating free fatty acids contribute to renal fibrosis and exacerbate insulin resistance.
Risk Factors for Diabetic Nephropathy with Severe Insulin Resistance
Several factors increase the likelihood of developing DN alongside severe insulin resistance:
- Obesity & Metabolic Syndrome: Excess visceral fat contributes to systemic insulin resistance and inflammatory cytokine release.
- Genetic Predisposition: Certain genetic markers increase susceptibility to both DN and insulin resistance.
- Hypertension: High blood pressure worsens renal damage by increasing glomerular capillary pressure.
- Dyslipidemia: Elevated LDL and triglycerides promote renal lipid deposition, aggravating nephropathy.
- Chronic Inflammation: Elevated inflammatory markers such as TNF-α and IL-6 accelerate renal fibrosis.
- Poor Glycemic Control: Chronic hyperglycemia intensifies oxidative stress and endothelial dysfunction.
Diagnosis and Biomarkers
1. Clinical Presentation
- Gradual onset of proteinuria (initially microalbuminuria, progressing to macroalbuminuria)
- Edema due to hypoalbuminemia
- Hypertension worsening over time
- Declining glomerular filtration rate (GFR)
2. Diagnostic Tests
| Test | Significance |
|---|---|
| Urinary Albumin-to-Creatinine Ratio (UACR) | Detects early proteinuria |
| Serum Creatinine & eGFR | Measures kidney function |
| Fasting Insulin & HOMA-IR | Assesses insulin resistance |
| Lipid Profile | Evaluates dyslipidemia |
| Cystatin C | Early marker of renal dysfunction |
| Inflammatory Markers (CRP, TNF-α, IL-6) | Identifies systemic inflammation |
Management Strategies
1. Glycemic Control
- SGLT2 Inhibitors: Reduce renal glucose reabsorption, lowering hyperglycemia and proteinuria.
- GLP-1 Receptor Agonists: Improve insulin sensitivity and promote weight loss.
- Metformin (Cautiously in CKD Patients): First-line for insulin resistance but requires dose adjustment in renal impairment.
- Insulin Therapy: Higher doses may be needed in severe insulin resistance, with careful monitoring to avoid hypoglycemia.
2. Blood Pressure Control
- ACE Inhibitors/ARBs: First-line for DN, reducing proteinuria and slowing progression.
- Mineralocorticoid Receptor Antagonists (MRA): Further reduce proteinuria when added to RAAS blockade.
3. Lipid and Inflammation Management
- Statins & PCSK9 Inhibitors: Lower LDL cholesterol and reduce cardiovascular risk.
- Anti-Inflammatory Agents (Pentoxifylline, Bardoxolone): Investigated for renoprotective effects.
4. Lifestyle Modifications
- Low-Protein, Low-Sodium Diet: Slows nephropathy progression while preventing metabolic acidosis.
- Exercise & Weight Loss: Improves insulin sensitivity and reduces kidney stress.
Advanced Therapies and Emerging Research
1. Renal Protective Agents
- Finerenone: A nonsteroidal mineralocorticoid receptor antagonist showing promise in reducing CKD progression.
- Endothelin Receptor Antagonists: Target renal fibrosis and vascular dysfunction.
2. Novel Insulin Sensitizers
- Thiazolidinediones (TZDs): Improve insulin sensitivity but have fluid retention risks.
- Berberine & Other Natural Compounds: Show potential in reducing insulin resistance and kidney inflammation.
3. Precision Medicine Approaches
- Genetic Screening for High-Risk Individuals: Enables early intervention.
- Targeted Anti-Inflammatory Therapies: Personalized treatment to counteract cytokine-induced renal damage.
Prognosis and Future Perspectives
Early detection and aggressive management significantly improve outcomes in DN with severe insulin resistance. The integration of novel pharmacologic therapies, lifestyle modifications, and precision medicine holds promise in slowing disease progression and enhancing quality of life. Future research aims to refine targeted treatments that address both insulin resistance and renal pathology at a molecular level.
MYHEALTHMAG