Diabetic macular edema (DME) is a leading cause of vision impairment among individuals with diabetes mellitus. The coexistence of DME and severe insulin resistance presents a complex clinical scenario, necessitating a comprehensive understanding of their interplay to inform effective management strategies.
Pathophysiology of Diabetic Macular Edema
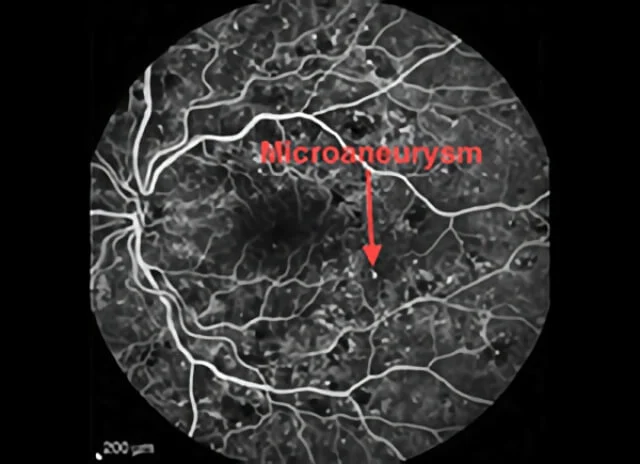
DME arises from the accumulation of fluid in the macula due to the breakdown of the blood-retinal barrier (BRB). Chronic hyperglycemia in diabetes leads to microvascular damage, resulting in increased vascular permeability. This process involves several key mechanisms:
- Hyperglycemia-Induced Damage: Elevated blood glucose levels cause biochemical alterations, including the accumulation of advanced glycation end products and activation of protein kinase C. These changes contribute to endothelial dysfunction and increased vascular permeability.
- Inflammatory Pathways: Chronic hyperglycemia induces inflammation, leading to the release of cytokines and growth factors such as vascular endothelial growth factor (VEGF). VEGF plays a pivotal role in increasing vascular permeability and promoting angiogenesis, exacerbating macular edema.
- Oxidative Stress: The imbalance between the production of reactive oxygen species and antioxidant defenses in diabetes results in oxidative stress, further damaging retinal cells and supporting the development of DME.
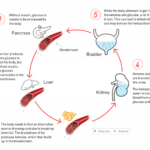
Insulin Resistance and Its Impact on DME
Insulin resistance, particularly in its severe form, significantly influences the progression of DME. The relationship between insulin resistance and DME can be delineated as follows:
- Hyperinsulinemia: To compensate for insulin resistance, the pancreas secretes higher levels of insulin. Elevated insulin levels have been associated with increased risk of DME, possibly due to insulin’s effects on retinal blood flow and vascular permeability.
- Metabolic Dysregulation: Insulin resistance contributes to poor glycemic control, dyslipidemia, and hypertension, all of which are established risk factors for the development and progression of DME.
- Inflammatory Mediators: Insulin resistance is linked to a pro-inflammatory state, characterized by elevated levels of cytokines and adipokines. This inflammatory milieu can exacerbate retinal vascular permeability and edema formation.
Risk Factors for DME in the Context of Severe Insulin Resistance
Several factors heighten the risk of developing DME in patients with severe insulin resistance:
- Duration of Diabetes: Prolonged duration of diabetes increases the likelihood of microvascular complications, including DME.
- Poor Glycemic Control: Elevated HbA1c levels correlate with a higher risk of DME, underscoring the importance of stringent blood glucose management.
- Hypertension: Elevated blood pressure exacerbates retinal vascular damage, contributing to the development of DME.
- Dyslipidemia: Abnormal lipid profiles, particularly elevated triglycerides and low HDL cholesterol, are associated with an increased risk of DME.
- Obesity: Excess adipose tissue contributes to insulin resistance and is an independent risk factor for DME.
Management Strategies for DME in Patients with Severe Insulin Resistance
Effective management of DME in the context of severe insulin resistance requires a multifaceted approach:
- Glycemic Control: Achieving and maintaining optimal blood glucose levels is paramount. This may involve lifestyle modifications, oral hypoglycemic agents, and insulin therapy. However, caution is warranted with insulin use, as some studies suggest an association between exogenous insulin therapy and increased risk of DME.
- Blood Pressure Management: Antihypertensive therapy should be optimized to maintain blood pressure within target ranges, thereby reducing the risk of retinal vascular complications.
- Lipid Management: Statin therapy and other lipid-lowering interventions can help achieve lipid targets, potentially mitigating the risk of DME.
- Pharmacotherapy for DME:
- Anti-VEGF Agents: Intravitreal injections of anti-VEGF agents (e.g., aflibercept, bevacizumab, ranibizumab) are first-line treatments for DME, effectively reducing macular thickness and improving visual acuity.
- Corticosteroids: Intravitreal corticosteroids may be considered, particularly in cases unresponsive to anti-VEGF therapy, though potential side effects such as cataract formation and elevated intraocular pressure must be monitored.
- Laser Photocoagulation: Focal or grid laser therapy may be employed as an adjunct to pharmacotherapy, particularly in cases with focal leakage observable on fluorescein angiography.
- Lifestyle Modifications: Weight loss, increased physical activity, and dietary changes can improve insulin sensitivity and contribute to overall metabolic control, potentially reducing the risk of DME progression.