Diabetic ketoacidosis (DKA) is a critical and potentially life-threatening complication predominantly associated with type 1 diabetes mellitus. It arises from a profound deficiency of insulin, leading to hyperglycemia, ketosis, and metabolic acidosis. The management of DKA typically involves insulin therapy to reverse the metabolic abnormalities. However, in certain patients, a condition known as severe insulin resistance complicates this treatment approach, necessitating significantly higher doses of insulin to achieve metabolic control. This article delves into the complex interplay between DKA and severe insulin resistance, exploring their pathophysiology, clinical manifestations, and advanced management strategies.
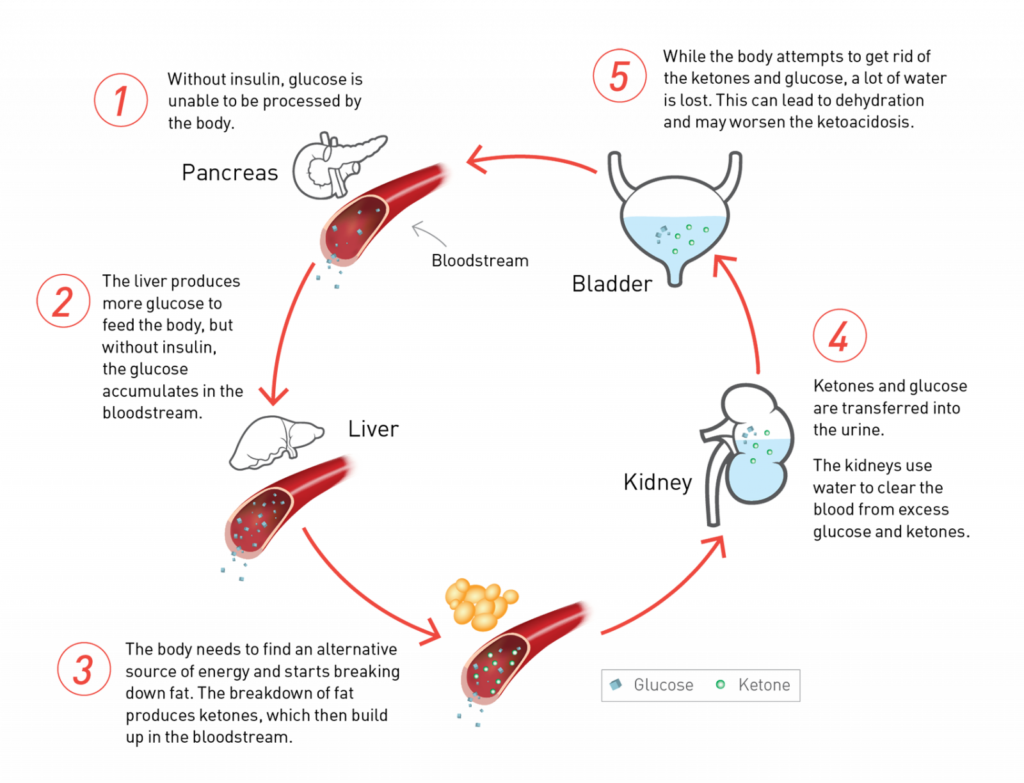
Pathophysiology of Diabetic Ketoacidosis
DKA develops due to an absolute or relative deficiency of insulin coupled with an increase in counter-regulatory hormones such as glucagon, cortisol, catecholamines, and growth hormone. This hormonal imbalance leads to increased hepatic glucose production through gluconeogenesis and glycogenolysis, while peripheral glucose utilization decreases. Concurrently, enhanced lipolysis results in elevated free fatty acids, which are converted in the liver to ketone bodies—acetoacetate and β-hydroxybutyrate—culminating in metabolic acidosis. The hallmark features of DKA include hyperglycemia, ketosis, and acidemia.
Understanding Severe Insulin Resistance
Severe insulin resistance is characterized by a markedly diminished response to both endogenous and exogenous insulin. Clinically, it is suspected when an individual requires insulin doses exceeding 2 units/kg/day to maintain euglycemia. Etiologies of severe insulin resistance encompass genetic mutations affecting the insulin receptor (as seen in conditions like Rabson-Mendenhall syndrome), autoimmune disorders producing insulin receptor antibodies (type B insulin resistance), and acquired conditions such as obesity and lipodystrophy.
Interrelation Between DKA and Severe Insulin Resistance
The coexistence of DKA and severe insulin resistance presents a formidable clinical challenge. In such scenarios, the standard insulin therapy protocols for DKA may prove inadequate, necessitating substantially higher insulin doses to overcome the resistance and achieve metabolic stabilization. This situation is particularly evident in patients with underlying conditions like type B insulin resistance syndrome, where autoantibodies against the insulin receptor impede insulin action, leading to extreme insulin requirements during DKA episodes.
Clinical Manifestations
Patients presenting with DKA and severe insulin resistance exhibit the classic symptoms of DKA, including polyuria, polydipsia, nausea, vomiting, abdominal pain, and altered mental status. Additionally, signs indicative of insulin resistance, such as acanthosis nigricans (a velvety hyperpigmentation of the skin), may be observed. In cases of autoimmune-mediated insulin resistance, features of concomitant autoimmune diseases, like systemic lupus erythematosus, might also be present.
Diagnostic Approach
The diagnosis of DKA is established through laboratory findings of hyperglycemia, ketonemia or ketonuria, and metabolic acidosis (low serum bicarbonate and arterial pH). In patients with suspected severe insulin resistance, further evaluation is warranted, including measurement of serum insulin levels, assessment for insulin receptor antibodies, and genetic testing for mutations in the insulin receptor gene. A thorough clinical assessment to identify physical stigmata of insulin resistance and associated conditions is also essential.
Management Strategies
Managing DKA in the context of severe insulin resistance requires a tailored approach:
- Insulin Therapy: High-dose intravenous insulin infusion is often necessary. Continuous monitoring of blood glucose and ketone levels guides therapy adjustments. In refractory cases, alternative therapies such as insulin-like growth factor 1 (IGF-1) have been explored, given its ability to activate insulin signaling pathways. nejm.org
- Fluid and Electrolyte Management: Aggressive fluid resuscitation with isotonic saline is critical to address dehydration. Electrolyte imbalances, particularly hypokalemia, should be promptly corrected, with careful monitoring to prevent complications.
- Identification and Treatment of Underlying Causes: Investigating and managing precipitating factors, such as infections or discontinuation of insulin therapy, are vital. In cases of autoimmune insulin resistance, immunosuppressive therapies may be considered to reduce antibody production.
- Adjunctive Therapies: Utilization of insulin sensitizers like metformin or thiazolidinediones may aid in reducing insulin resistance, though their use should be judicious and individualized.
Prognosis and Follow-Up
The prognosis of patients with DKA and severe insulin resistance varies based on the underlying etiology and the promptness of management. Early recognition and aggressive treatment are pivotal in improving outcomes. Long-term management includes regular follow-up to monitor glycemic control, assessment for potential complications, and ongoing evaluation of insulin requirements. Patient education on adherence to therapy and lifestyle modifications plays a crucial role in preventing recurrence.