Diabetic gastroparesis is a serious complication of long-standing diabetes, characterized by delayed gastric emptying without mechanical obstruction. It frequently coexists with severe insulin resistance, creating a difficult cycle of unpredictable blood glucose fluctuations and worsening gastrointestinal symptoms. This condition significantly impacts both glycemic control and quality of life, necessitating a comprehensive and individualized treatment approach.
Pathophysiology of Diabetic Gastroparesis
Autonomic Neuropathy and Gastric Dysfunction
Chronic hyperglycemia leads to autonomic neuropathy, particularly affecting the vagus nerve, which is responsible for regulating stomach contractions. When the vagus nerve is damaged, the coordinated movement of gastric muscles is impaired, leading to slow or incomplete emptying of food from the stomach. Additionally, hyperglycemia damages blood vessels that supply oxygen and nutrients to gastric nerves, further exacerbating motility issues.
Role of Interstitial Cells of Cajal
The interstitial cells of Cajal (ICCs) act as pacemakers within the gastrointestinal tract, ensuring smooth and rhythmic contractions. In diabetic gastroparesis, a significant loss or dysfunction of these cells occurs, leading to disorganized gastric motility and prolonged gastric retention.
Severe Insulin Resistance in Diabetic Gastroparesis
Mechanisms of Insulin Resistance
Insulin resistance in diabetic gastroparesis arises from multiple factors, including:
- Chronic hyperglycemia, which downregulates insulin receptor sensitivity.
- Increased free fatty acids, leading to impaired glucose uptake in muscle and liver cells.
- Inflammatory mediators, which interfere with insulin signaling pathways.
This insulin resistance, combined with delayed gastric emptying, creates unpredictable postprandial glucose levels, making diabetes management exceptionally difficult.
Impact on Glycemic Control
The irregular absorption of nutrients caused by delayed gastric emptying leads to erratic blood glucose spikes and drops. Patients may experience:
- Hyperglycemia due to delayed insulin action when food is retained in the stomach.
- Hypoglycemia when insulin is absorbed before food leaves the stomach.
- Increased variability in glucose readings, making insulin dosing challenging.
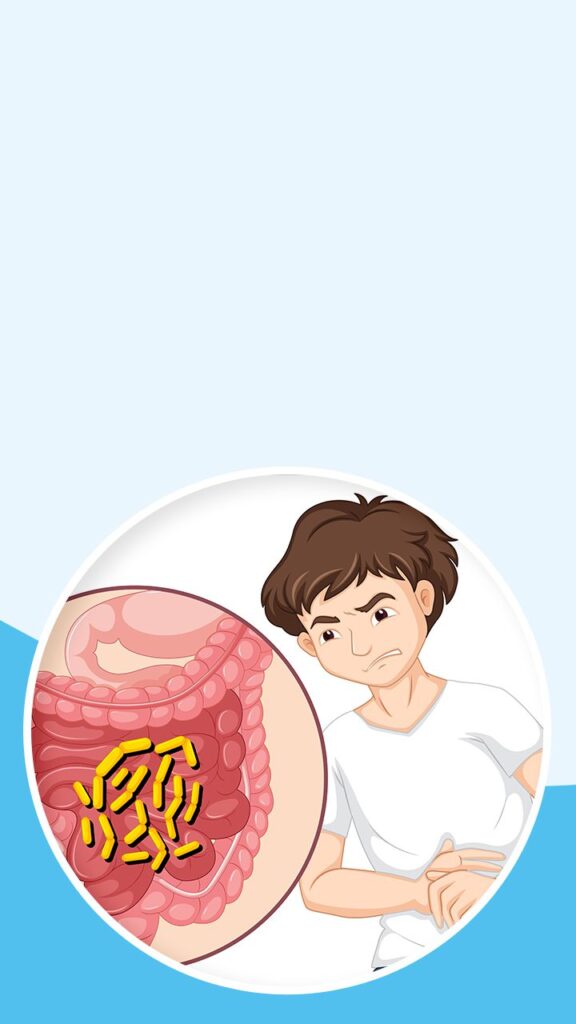
Clinical Manifestations
Diabetic gastroparesis with severe insulin resistance presents with a range of symptoms, including:
- Nausea and vomiting, particularly after meals.
- Early satiety, with an inability to finish normal portions.
- Bloating and abdominal discomfort due to prolonged food retention.
- Erratic blood glucose levels, which are difficult to manage with standard insulin regimens.
These symptoms significantly impact nutritional intake, weight maintenance, and overall metabolic stability.
Diagnostic Approaches
Gastric Emptying Scintigraphy
This gold-standard test evaluates the rate at which food leaves the stomach using a radiolabeled meal and imaging techniques. A delayed gastric emptying time confirms gastroparesis.
Additional Diagnostic Tools
- Gastric manometry to assess stomach muscle contractions.
- Upper endoscopy to rule out mechanical obstructions.
- Wireless motility capsule to evaluate the passage of food through the digestive tract.
Management Strategies
Glycemic Control
- Frequent blood glucose monitoring to detect erratic patterns.
- Insulin therapy adjustments, including changes in dosing and timing to match delayed nutrient absorption.
- Use of continuous glucose monitoring (CGM) for real-time blood glucose tracking.
Dietary Modifications
- Small, frequent meals to minimize gastric workload.
- Low-fat, low-fiber diets to prevent further delays in gastric emptying.
- Liquid-based nutrition for better gastric transit and improved absorption.
Pharmacological Interventions
- Prokinetic agents to enhance gastric motility, such as metoclopramide and domperidone.
- Antiemetic medications to control nausea and vomiting.
- GLP-1 receptor agonists, though controversial, may have some benefit in certain cases.
Advanced Therapies
- Gastric electrical stimulation (GES) to regulate stomach contractions and reduce symptoms.
- Jejunostomy feeding tubes for severe cases where oral intake is inadequate.
- Botulinum toxin injections to relax the pyloric sphincter and improve gastric emptying.