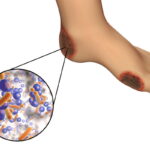
Diabetic foot infections (DFIs) represent a significant complication in individuals with diabetes, particularly those experiencing severe insulin resistance. The interplay between impaired glucose metabolism and vascular insufficiency exacerbates the susceptibility to infections, posing substantial challenges in clinical management.

Pathophysiology of Diabetic Foot Infections
DFIs typically arise from a combination of factors:
- Neuropathy: Chronic hyperglycemia leads to peripheral neuropathy, diminishing sensory perception and increasing the risk of unnoticed injuries.
- Peripheral Arterial Disease (PAD): Diabetes accelerates atherosclerosis, reducing blood flow and impairing wound healing.
- Immunosuppression: Elevated blood glucose levels compromise immune responses, facilitating bacterial proliferation.
In the context of severe insulin resistance, these factors are often intensified, leading to a higher propensity for infection and delayed recovery.
Risk Factors Associated with Severe Insulin Resistance
Individuals with pronounced insulin resistance may exhibit:
- Poor Glycemic Control: Elevated HbA1c levels correlate with increased infection rates.
- Obesity: Excess adipose tissue contributes to both mechanical stress on the feet and systemic inflammation.
- Dyslipidemia: Abnormal lipid profiles exacerbate vascular complications, further impeding blood flow to extremities.
Clinical Manifestations
DFIs can present with a spectrum of symptoms, including:
- Local Signs: Erythema, warmth, swelling, and purulent discharge.
- Systemic Signs: Fever, chills, and leukocytosis in severe cases.
- Complications: Progression to osteomyelitis or necrotizing fasciitis if not promptly addressed.
Diagnostic Approach
A thorough evaluation encompasses:
- Clinical Assessment: Detailed examination of the affected area, noting the extent and depth of the infection.
- Imaging Studies: Utilization of radiographs or MRI to assess for underlying osteomyelitis.
- Microbiological Cultures: Obtaining deep tissue samples to identify causative pathogens and guide antibiotic therapy.
Management Strategies
Effective management of DFIs in the setting of severe insulin resistance involves:
- Glycemic Optimization: Intensive insulin therapy to achieve target blood glucose levels.
- Antibiotic Therapy: Empirical broad-spectrum antibiotics, tailored based on culture results.
- Surgical Intervention: Debridement of necrotic tissue or drainage of abscesses as indicated.
- Offloading Techniques: Use of specialized footwear or devices to reduce pressure on affected areas.
- Vascular Assessment: Evaluation and management of PAD, potentially involving revascularization procedures.
Prevention of Diabetic foot infection
Preventive measures are paramount and include:
- Regular Foot Examinations: Routine inspections by healthcare providers and patient self-examinations.
- Patient Education: Instruction on proper foot care, including hygiene and nail care.
- Lifestyle Modifications: Encouraging weight management, smoking cessation, and regular physical activity to improve insulin sensitivity.