Diabetes mellitus encompasses a group of metabolic disorders characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Severe insulin resistance represents a significant challenge in the management of diabetes, as it impairs the body’s ability to utilize insulin effectively, leading to elevated blood glucose levels and associated complications.
Understanding Severe Insulin Resistance
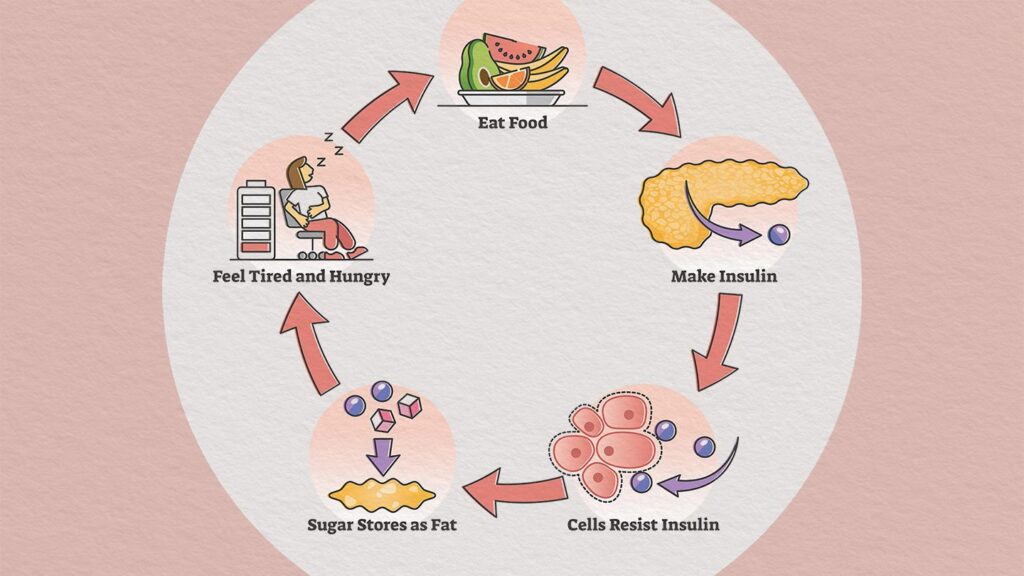
Insulin resistance occurs when cells in the muscles, fat, and liver fail to respond adequately to insulin, a hormone that facilitates glucose uptake from the bloodstream into cells. In severe cases, this resistance is profound, necessitating substantially higher insulin levels to maintain normoglycemia. This condition is often associated with genetic mutations affecting the insulin receptor or post-receptor signaling pathways.
Pathophysiology of diabetes mellitus with severe insulin resistance
In individuals with severe insulin resistance, the impaired response to insulin leads to decreased glucose uptake by peripheral tissues and increased hepatic glucose production. The pancreas compensates by secreting more insulin, resulting in hyperinsulinemia. Over time, this compensatory mechanism may fail, leading to persistent hyperglycemia and the development of type 2 diabetes mellitus.
Causes of Severe Insulin Resistance
Several factors contribute to the development of severe insulin resistance:
- Genetic Mutations: Mutations in the insulin receptor gene (INSR) can lead to conditions such as Donohue syndrome and Rabson-Mendenhall syndrome, characterized by extreme insulin resistance from birth.
- Obesity: Excess adipose tissue, particularly visceral fat, releases pro-inflammatory cytokines and free fatty acids that interfere with insulin signaling pathways.
- Sedentary Lifestyle: Lack of physical activity reduces insulin sensitivity, as muscle contractions during exercise enhance glucose uptake independent of insulin.
- Hormonal Disorders: Conditions like Cushing’s syndrome and acromegaly involve excess hormones that antagonize insulin action, contributing to insulin resistance.
Clinical Manifestations
Patients with severe insulin resistance may present with:
- Acanthosis Nigricans: Dark, velvety patches of skin, typically in body folds and creases, indicating high insulin levels.
- Hyperglycemia: Elevated blood glucose levels leading to symptoms such as polyuria, polydipsia, and unexplained weight loss.
- Dyslipidemia: Abnormal lipid profiles, including elevated triglycerides and decreased HDL cholesterol.
- Hypertension: Increased blood pressure, commonly associated with insulin resistance and metabolic syndrome.
Diagnostic Evaluation
The assessment of severe insulin resistance involves:
- Fasting Insulin and Glucose Levels: Elevated fasting insulin levels alongside normal or elevated glucose levels suggest insulin resistance.
- Oral Glucose Tolerance Test (OGTT): Measures the body’s response to glucose intake, with prolonged hyperglycemia indicating impaired glucose tolerance.
- Genetic Testing: Identifies mutations in the INSR gene or other related genes in suspected congenital cases.
Management Strategies
Effective management of severe insulin resistance requires a multifaceted approach:
Lifestyle Modifications
- Dietary Interventions: Emphasize a balanced diet rich in fiber, whole grains, lean proteins, and healthy fats while limiting refined carbohydrates and saturated fats.
- Physical Activity: Regular aerobic and resistance exercises enhance insulin sensitivity and promote weight loss.
Pharmacological Therapies
- Insulin Sensitizers: Medications such as metformin and thiazolidinediones improve insulin sensitivity by enhancing glucose uptake and reducing hepatic glucose production.
- High-Dose Insulin Therapy: In cases where endogenous insulin production is insufficient, exogenous insulin may be administered in higher doses to overcome resistance.
- Emerging Therapies: Research into agents targeting specific molecular pathways involved in insulin signaling is ongoing, offering potential future treatment options.
Surgical Interventions
- Bariatric Surgery: For individuals with morbid obesity, surgical procedures like gastric bypass can lead to significant weight loss and improvement in insulin sensitivity.
Prognosis and Complications
Without effective management, severe insulin resistance can lead to:
- Type 2 Diabetes Mellitus: Persistent hyperglycemia resulting from insulin resistance.
- Cardiovascular Disease: Increased risk due to associated hypertension and dyslipidemia.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Accumulation of fat in the liver, potentially progressing to cirrhosis.

