Diabetes insipidus is a rare condition characterized by an imbalance in the body’s ability to regulate fluids, leading to excessive urination (polyuria) and increased thirst (polydipsia). Unlike diabetes mellitus, which is associated with high blood sugar levels, diabetes insipidus is caused by issues related to the production, release, or response to antidiuretic hormone (ADH), also known as vasopressin.
Types of Diabetes Insipidus
Diabetes insipidus has four primary types, each with distinct causes and mechanisms:
1. Central Diabetes Insipidus (CDI)
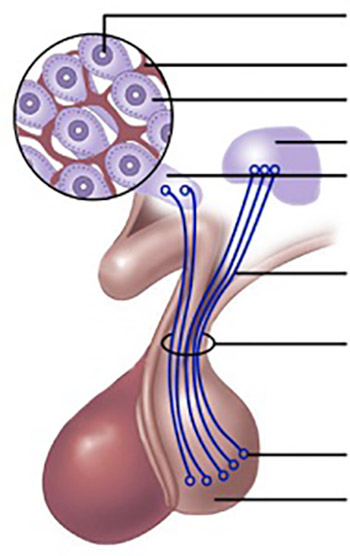
Central diabetes insipidus, also called arginine vasopressin deficiency (AVP-D), occurs due to insufficient production or release of ADH from the hypothalamus or pituitary gland. This leads to excessive water loss through the kidneys.
Causes of CDI:
- Idiopathic (unknown origin)
- Head trauma
- Brain tumors affecting the pituitary gland
- Neurosurgical interventions
- Infections or inflammatory diseases (e.g., meningitis, encephalitis, sarcoidosis)
2. Nephrogenic Diabetes Insipidus (NDI)
Also known as arginine vasopressin resistance (AVP-R), this form occurs when the kidneys fail to respond to ADH, preventing water reabsorption.
Causes of NDI:
- Genetic mutations affecting kidney function
- Chronic kidney disease
- Lithium toxicity
- Electrolyte imbalances (hypercalcemia or hypokalemia)
- Certain medications
3. Dipsogenic Diabetes Insipidus
This form is caused by a defect in the hypothalamic thirst mechanism, leading to excessive fluid intake and suppression of ADH release.
Causes of Dipsogenic DI:
- Hypothalamic damage from trauma, surgery, or tumors
- Psychiatric disorders that affect thirst perception
4. Gestational Diabetes Insipidus
A rare condition occurring during pregnancy, gestational diabetes insipidus results from the placenta producing an enzyme (vasopressinase) that degrades ADH. It typically resolves after childbirth but requires management during pregnancy.
Causes and Risk Factors
The causes of diabetes insipidus vary based on type:
- Central DI: Damage to the hypothalamus or pituitary gland due to surgery, tumors, infections, or trauma.
- Nephrogenic DI: Kidney dysfunction caused by genetics, medications (especially lithium), chronic kidney disease, or metabolic imbalances.
- Dipsogenic DI: Dysfunction of the hypothalamic thirst center due to injury, inflammation, or psychological factors.
- Gestational DI: Increased production of vasopressinase by the placenta, leading to ADH degradation.
Symptoms
The hallmark symptoms of diabetes insipidus include:
- Excessive Thirst (Polydipsia): A strong urge to drink large amounts of water.
- Frequent Urination (Polyuria): The passage of large volumes of dilute urine.
- Nocturia: Frequent urination during the night.
- Dehydration: In severe cases, leading to dry skin, fatigue, and dizziness.
- Electrolyte Imbalances: Potential disturbances in sodium and potassium levels.
In extreme cases, individuals may produce up to 20 liters of urine per day.
Diagnosis
Diagnosis of diabetes insipidus involves several tests:
1. Water Deprivation Test
A controlled test assessing the body’s ability to concentrate urine when deprived of fluids. It helps differentiate between various forms of DI.
2. Desmopressin Stimulation Test
A synthetic ADH (desmopressin) is administered to evaluate the kidneys’ response. Improvement in urine concentration indicates central DI, while no response suggests nephrogenic DI.
3. Magnetic Resonance Imaging (MRI)
Used to detect abnormalities in the hypothalamus or pituitary gland, such as tumors or structural damage.
4. Blood Tests
Checks for electrolyte imbalances and kidney function markers.
Treatment
1. Central Diabetes Insipidus Treatment
- Desmopressin (DDAVP): A synthetic ADH replacement available as a nasal spray, oral tablet, or injection.
- Hydration: Maintaining adequate fluid intake to prevent dehydration.
2. Nephrogenic Diabetes Insipidus Treatment
- Discontinuation of Lithium or Other Causative Drugs: If applicable.
- Dietary Modifications: Low-salt, low-protein diet to reduce urine output.
- Thiazide Diuretics & NSAIDs: Medications that help concentrate urine and reduce symptoms.
3. Dipsogenic Diabetes Insipidus Treatment
- Behavioral Therapy: Techniques to regulate fluid intake.
- Management of Underlying Conditions: Treatment for hypothalamic damage or psychiatric disorders.
4. Gestational Diabetes Insipidus Treatment
- Desmopressin: The preferred treatment to compensate for ADH degradation.
Complications of Diabetes Insipidus
If left untreated, diabetes insipidus can lead to:
- Severe Dehydration: Resulting in dry skin, confusion, low blood pressure, and dizziness.
- Electrolyte Imbalances: Affecting sodium and potassium levels, potentially leading to muscle weakness, seizures, and heart issues.
- Chronic Fatigue and Sleep Disturbances: Due to frequent urination and dehydration.
Preventive Measures
Although diabetes insipidus cannot always be prevented, certain measures can help manage risks:
- Avoid Medications That Cause Nephrogenic DI: Regular monitoring for individuals taking lithium or other nephrotoxic drugs.
- Proper Management of Head Injuries or Neurosurgical Conditions: Reducing the risk of pituitary damage.
- Regular Medical Checkups: Early detection and treatment of conditions affecting kidney or hypothalamic function.

