Desmoid tumors, also known as aggressive fibromatosis, are rare, locally invasive soft tissue tumors arising from connective tissue. While they do not metastasize, their aggressive local infiltration can cause significant morbidity. These tumors can develop anywhere in the body but commonly affect the abdominal wall, extremities, and intra-abdominal regions.
Epidemiology and Risk Factors
Desmoid tumors are uncommon, with an estimated incidence of 5 to 6 cases per million people annually. They most frequently occur in individuals aged 15 to 60 years, with a higher prevalence in females. Several key factors contribute to their development:
1. Genetic Mutations
- CTNNB1 Gene Mutation: Most sporadic desmoid tumors result from mutations in the CTNNB1 gene, leading to abnormal β-catenin accumulation.
- APC Gene Mutation: Patients with familial adenomatous polyposis (FAP), particularly those with Gardner’s syndrome, have an increased risk due to APC gene mutations.
2. Hormonal Influence
- Estrogen has been linked to desmoid tumor development, which explains the increased incidence in women, especially during or after pregnancy.
3. Trauma and Surgical History
- Physical trauma, including surgical procedures, is a potential trigger, particularly in genetically predisposed individuals.
4. Prior Radiation Exposure
- Some cases have been linked to previous radiation therapy, though this is less common.
Clinical Presentation of Desmoid Tumors
The symptoms of desmoid tumors vary depending on tumor location, size, and degree of invasion.
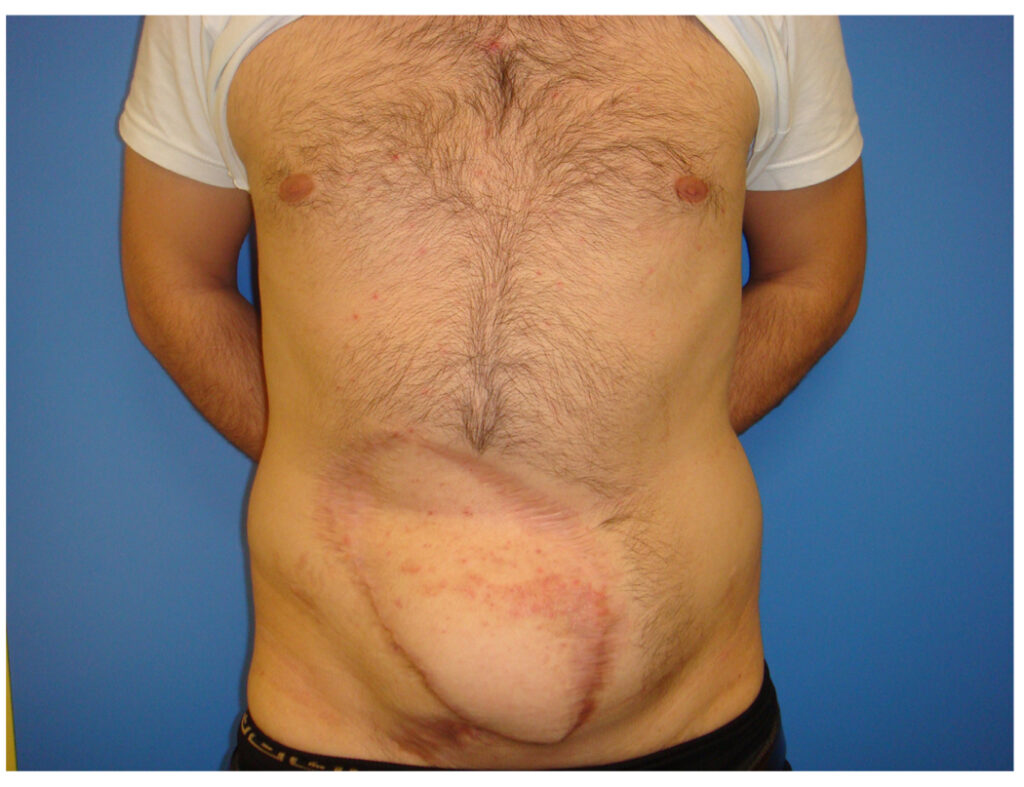
1. Abdominal Wall Desmoid Tumors
- Typically present as a firm, painless mass.
- May gradually increase in size without significant symptoms.
2. Intra-Abdominal Desmoid Tumors
- More common in individuals with FAP.
- Can cause abdominal pain, bowel obstruction, nausea, and vomiting due to compression of internal organs.
3. Extra-Abdominal Desmoid Tumors
- Frequently occur in the shoulder girdle, chest wall, and extremities.
- Can lead to pain, swelling, restricted movement, and functional impairment.
4. Complications
- Desmoid tumors can compress nerves, blood vessels, and internal organs, leading to significant complications despite their benign classification.
Diagnosis of Desmoid Tumors
1. Imaging Studies
- Magnetic Resonance Imaging (MRI) is the preferred imaging modality, providing detailed insights into tumor size, margins, and infiltration.
- Computed Tomography (CT) scans are useful for evaluating intra-abdominal desmoid tumors.
2. Histopathological Examination
- Core needle biopsy is essential for definitive diagnosis.
- Tumors show spindle-shaped fibroblastic cells embedded in collagen-rich tissue.
3. Immunohistochemistry
- β-catenin nuclear staining is a key diagnostic marker, distinguishing desmoid tumors from other soft tissue neoplasms.
Treatment Options for Desmoid Tumors
The management of desmoid tumors depends on tumor location, progression, symptoms, and patient preference.
1. Active Surveillance (“Watch and Wait”)
- Many desmoid tumors exhibit spontaneous regression or remain stable.
- Regular MRI or CT scans are performed to monitor tumor progression.
2. Surgery
- Historically considered the first-line treatment, but due to high recurrence rates (20-80%), it is now reserved for symptomatic cases.
- Surgical excision aims for negative margins, but aggressive resection may cause functional impairment.
3. Systemic Therapies
a. Hormonal and Anti-Inflammatory Agents
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as celecoxib, may help slow tumor growth.
- Selective estrogen receptor modulators (SERMs) like tamoxifen are used, particularly in estrogen-driven tumors.
b. Chemotherapy and Targeted Therapy
- Tyrosine kinase inhibitors (TKIs) such as sorafenib and pazopanib have shown efficacy in cases of progressive disease.
- Nirogacestat, a gamma-secretase inhibitor, received FDA approval in 2023 as a breakthrough treatment for desmoid tumors, demonstrating significant tumor shrinkage.
c. Radiation Therapy
- Considered for unresectable or recurrent tumors, particularly in patients where surgery is not viable.
Prognosis and Long-Term Outlook
1. Risk of Recurrence
- Desmoid tumors have a high recurrence rate, particularly after surgery.
- Recurrence is more likely in younger patients, incompletely resected tumors, and intra-abdominal locations.
2. Survival Rate
- Since desmoid tumors are benign and non-metastatic, overall survival rates are excellent.
- However, aggressive cases can significantly impact quality of life due to pain, functional limitations, and complications.
3. Ongoing Monitoring
- Long-term follow-up with regular imaging and clinical evaluations is necessary, especially for patients who have undergone treatment.