Dermatomyositis is a rare autoimmune inflammatory disease that primarily affects the skin and muscles. It is categorized under idiopathic inflammatory myopathies and is marked by muscle weakness and characteristic skin manifestations. The condition can develop at any age, but it is most common in adults between 40 and 60 years and children aged 5 to 15. Women are more frequently affected than men.
Clinical Manifestations
Skin Involvement
The dermatological symptoms of dermatomyositis are distinctive and often precede muscle weakness:
- Heliotrope Rash: A violet or dusky discoloration around the eyes, often accompanied by swelling.
- Gottron’s Papules: Raised, scaly, red or violaceous plaques found over the knuckles, elbows, or knees.
- Shawl Sign: A widespread rash covering the upper back, shoulders, and chest.
- V-Sign: A rash in a V-shaped pattern over the anterior chest.
- Mechanic’s Hands: Thickened, cracked, and roughened skin on the sides of the fingers and palms.
Muscle Involvement
Dermatomyositis is characterized by progressive and symmetrical muscle weakness that primarily affects proximal muscles:
- Proximal Muscle Weakness: Difficulty climbing stairs, rising from a seated position, lifting objects, or reaching overhead.
- Dysphagia: Swallowing difficulties due to involvement of the esophageal muscles.
- Respiratory Complications: Weakness in respiratory muscles may lead to breathing difficulties and respiratory failure in severe cases.

Etiology and Pathogenesis
The exact cause of dermatomyositis remains unknown, but several factors contribute to its development:
- Autoimmune Dysfunction: The immune system mistakenly attacks muscle and skin tissues, leading to chronic inflammation.
- Genetic Susceptibility: Certain genetic markers are associated with an increased risk of developing dermatomyositis.
- Environmental Triggers: Viral infections, medications, and exposure to ultraviolet radiation have been proposed as triggers for disease onset.
Associated Conditions
Dermatomyositis is often linked to other medical conditions, particularly in adults:
- Malignancy: Up to 15% of adult cases are associated with cancers, including ovarian, lung, breast, and gastrointestinal cancers.
- Interstitial Lung Disease (ILD): Inflammation of the lungs can cause respiratory impairment and chronic pulmonary complications.
- Calcinosis: Deposits of calcium under the skin, leading to painful nodules, particularly in juvenile dermatomyositis.
Diagnostic Evaluation
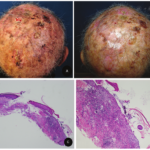
Diagnosis of dermatomyositis is based on clinical findings, laboratory tests, imaging studies, and histopathology:
- Clinical Examination: Assessment of characteristic skin rashes and proximal muscle weakness.
- Laboratory Tests: Elevated muscle enzymes, including creatine kinase (CK) and aldolase, indicate muscle damage.
- Autoantibody Panel: Myositis-specific autoantibodies, such as anti-Mi-2, anti-TIF1-γ, and anti-NXP2, help confirm diagnosis and assess prognosis.
- Electromyography (EMG): Detects abnormal muscle electrical activity, supporting the diagnosis of inflammatory myopathy.
- Magnetic Resonance Imaging (MRI): Identifies muscle inflammation and damage.
- Muscle and Skin Biopsy: Confirms histopathological features of dermatomyositis, including perivascular inflammation and muscle fiber degeneration.
Management Strategies
Dermatomyositis treatment aims to reduce inflammation, improve muscle function, and prevent complications.
Pharmacologic Treatment
- Corticosteroids: First-line treatment to reduce inflammation and improve symptoms.
- Immunosuppressive Agents: Methotrexate, azathioprine, or mycophenolate mofetil are used to control disease progression in steroid-resistant cases.
- Intravenous Immunoglobulin (IVIG): Beneficial for refractory cases, especially in patients with severe muscle weakness.
- Biologic Therapies: Emerging treatments, such as rituximab, target B cells to modulate immune response.
Supportive Therapies
- Physical Therapy: Helps maintain muscle strength and mobility.
- Speech and Swallowing Therapy: Assists in managing dysphagia and preventing aspiration pneumonia.
- Sun Protection: Due to photosensitivity, patients should use broad-spectrum sunscreen and wear protective clothing.
Monitoring and Long-Term Management
- Regular Cancer Screening: Given the strong association with malignancies, routine screening is recommended.
- Pulmonary Function Monitoring: Necessary in patients with interstitial lung disease to prevent respiratory complications.
Prognosis
The prognosis of dermatomyositis varies based on disease severity and response to treatment:
- Complete Remission: Some patients achieve remission with early and aggressive treatment.
- Chronic Disease Course: Others may experience persistent symptoms requiring long-term immunosuppression.
- Complications: Severe cases can result in muscle atrophy, pulmonary fibrosis, and increased mortality due to malignancies.