Acute ST elevation myocardial infarction (STEMI) is a severe and life-threatening type of heart attack caused by the complete blockage of a coronary artery. This leads to myocardial ischemia and necrosis, demanding immediate medical intervention to restore blood flow and prevent fatal complications. Advances in cardiology have significantly improved STEMI outcomes through early diagnosis, rapid revascularization, and comprehensive post-event management.
Pathophysiology of STEMI
STEMI occurs due to the rupture of an atherosclerotic plaque within a coronary artery, triggering thrombus formation. The obstruction leads to myocardial ischemia, infarction, and, if untreated, irreversible myocardial damage.
Risk Factors
Several factors contribute to the development of STEMI, including:
- Hypertension: Chronic high blood pressure damages arterial walls.
- Hyperlipidemia: Elevated LDL cholesterol accelerates plaque buildup.
- Diabetes Mellitus: Increases endothelial dysfunction and atherosclerosis.
- Smoking: Causes oxidative stress and vascular inflammation.
- Obesity: Associated with metabolic syndrome and cardiovascular disease.
- Sedentary Lifestyle: Reduces cardiovascular fitness and increases risk.
- Family History: Genetic predisposition to coronary artery disease (CAD).
Clinical Symptoms
Patients with STEMI typically present with:
- Severe Chest Pain: Intense, persistent retrosternal pain radiating to the left arm, jaw, or back.
- Dyspnea: Shortness of breath due to impaired cardiac function.
- Diaphoresis: Profuse sweating triggered by sympathetic activation.
- Nausea and Vomiting: Vagal stimulation due to myocardial injury.
- Palpitations: Arrhythmias caused by ischemic myocardium.
Diagnosis
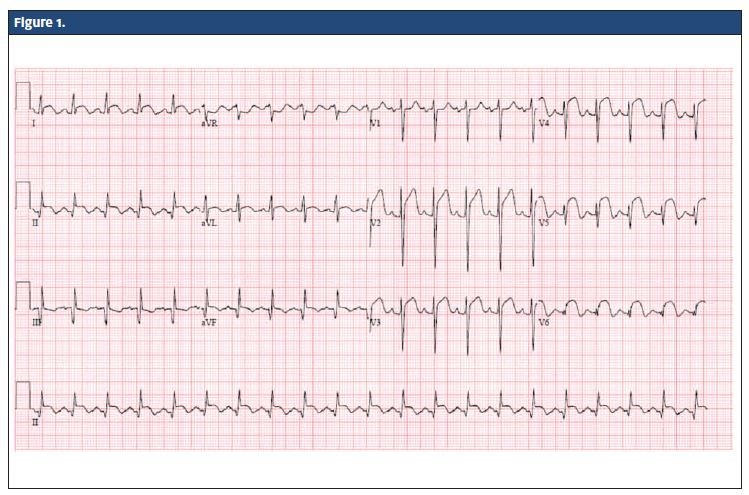
1. Electrocardiogram (ECG)
- ST-segment elevation in at least two contiguous leads.
- Reciprocal ST depression in opposing leads.
- Pathological Q waves may develop later.
2. Cardiac Biomarkers
- Troponin I/T: Elevated levels indicate myocardial injury.
- Creatine Kinase-MB (CK-MB): Confirms infarction severity.
3. Echocardiography
- Identifies regional wall motion abnormalities.
- Assesses left ventricular function.
4. Coronary Angiography
- Locates the site of arterial occlusion.
- Determines the need for percutaneous coronary intervention (PCI).
Treatment Strategies
1. Reperfusion Therapy
- Percutaneous Coronary Intervention (PCI): Preferred strategy for restoring coronary flow.
- Thrombolysis: Used when PCI is unavailable, utilizing fibrinolytic agents (e.g., alteplase, tenecteplase).
2. Adjunctive Pharmacotherapy
- Antiplatelet Agents: Aspirin and P2Y12 inhibitors (clopidogrel, ticagrelor) to prevent further thrombus formation.
- Anticoagulants: Heparin or enoxaparin to reduce clot propagation.
- Beta-blockers: Reduce myocardial oxygen demand.
- ACE Inhibitors/ARBs: Prevent cardiac remodeling and heart failure.
- Statins: Lower LDL cholesterol and stabilize plaques.
3. Supportive Care
- Oxygen Therapy: Administered in hypoxemic patients.
- Pain Management: Morphine for pain relief and anxiety reduction.
- Cardiac Monitoring: Continuous ECG to detect arrhythmias.
Prevention Strategies
- Lifestyle Modifications: Smoking cessation, healthy diet, regular exercise.
- Blood Pressure and Lipid Control: Strict management of hypertension and dyslipidemia.
- Diabetes Management: Glycemic control to prevent vascular damage.
- Regular Health Screenings: Early detection of cardiovascular risk factors.
Prognosis and Complications
Timely intervention significantly improves STEMI prognosis. However, untreated or delayed management can lead to:
- Heart Failure: Due to extensive myocardial damage.
- Arrhythmias: Life-threatening ventricular tachycardia or fibrillation.
- Cardiogenic Shock: Severe left ventricular dysfunction leading to organ failure.
- Mechanical Complications: Papillary muscle rupture, ventricular septal defect.
Acute ST-elevation myocardial infarction is a medical emergency requiring rapid diagnosis and intervention. Advances in reperfusion therapy, pharmacological management, and preventive strategies have significantly improved patient outcomes. Public awareness and early recognition of symptoms remain critical in reducing STEMI-related morbidity and mortality.