Parkinson’s disease (PD) is primarily recognized for its motor symptoms, such as tremors, muscle rigidity, and bradykinesia. However, a significant portion of individuals with PD also develop cognitive decline, culminating in a condition known as Parkinson’s disease dementia (PDD). This article provides a comprehensive overview of PDD, including its symptoms, causes, diagnosis, and management strategies.
What is Parkinson’s Disease Dementia?
Parkinson’s disease dementia is a progressive neurological disorder that affects cognition, memory, and executive function. It typically develops in individuals who have had Parkinson’s disease for several years, with cognitive symptoms emerging at least one year after the onset of motor symptoms. The condition significantly impacts daily functioning, leading to increased caregiver burden and reduced quality of life.
Key Differences: Parkinson’s Disease Dementia vs. Dementia with Lewy Bodies
Both PDD and Dementia with Lewy Bodies (DLB) share similarities due to the presence of Lewy body pathology. However, they differ in the sequence of symptom onset:
- PDD: Cognitive symptoms appear at least a year after Parkinson’s motor symptoms.
- DLB: Cognitive decline occurs before or concurrently with motor symptoms.
Symptoms of Parkinson’s Disease Dementia
Cognitive Symptoms
- Impaired attention and concentration
- Executive dysfunction (difficulty with planning and problem-solving)
- Visuospatial difficulties (trouble judging distances or recognizing objects)
- Memory impairment (retrieval issues rather than encoding problems)
- Language difficulties, including slowed speech
Behavioral and Psychological Symptoms
- Depression and anxiety
- Apathy and lack of motivation
- Visual hallucinations and delusions
- Sleep disturbances, including REM sleep behavior disorder
Motor Symptoms
- Increased muscle rigidity
- Worsening bradykinesia
- Postural instability and frequent falls
Causes and Risk Factors
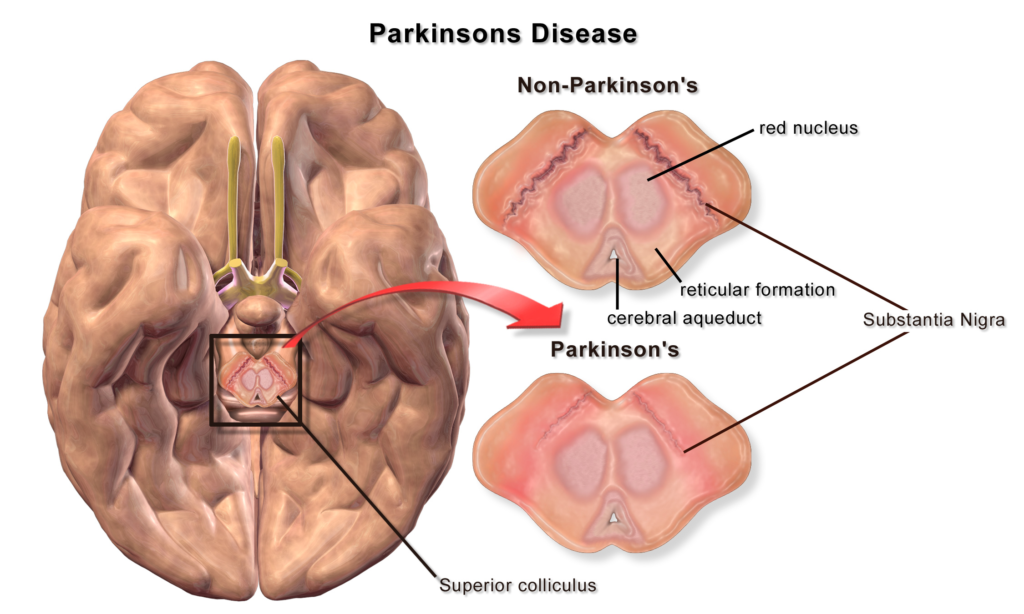
The exact cause of Parkinson’s disease dementia is not fully understood, but several factors contribute to its development:
Neuropathological Mechanisms
- Lewy Bodies: Abnormal protein deposits (alpha-synuclein) accumulate in neurons, disrupting brain function.
- Neurotransmitter Imbalance: Dopamine depletion affects motor function, while acetylcholine deficits contribute to cognitive decline.
- Cerebral Atrophy: Brain shrinkage, particularly in the frontal and temporal lobes, correlates with cognitive symptoms.
Risk Factors
- Advanced age
- Longer disease duration
- Severe motor symptoms
- Presence of hallucinations or REM sleep behavior disorder
- Genetic predisposition (mutations in SNCA, LRRK2, and GBA genes)
Diagnosis of Parkinson’s Disease Dementia
Diagnostic Criteria
PDD is diagnosed based on clinical symptoms and neurological assessments. Physicians typically use:
- Medical History & Symptom Timeline: To distinguish PDD from other dementias.
- Neurocognitive Testing: Assessing memory, executive function, and visuospatial skills.
- Brain Imaging: MRI or PET scans to rule out other causes of cognitive decline.
- Biomarkers: Emerging research suggests cerebrospinal fluid (CSF) and blood markers may aid diagnosis in the future.
Differentiating PDD from Other Forms of Dementia
The following table highlights the distinctions between PDD, Alzheimer’s disease (AD), and DLB:
| Feature | PDD | Alzheimer’s Disease | DLB |
|---|---|---|---|
| Onset of Dementia | After motor symptoms | Early memory loss | Concurrent with or before motor symptoms |
| Hallucinations | Common | Rare | Very common |
| Memory Impairment | Retrieval deficits | Encoding deficits | Variable |
| Response to L-Dopa | Improves motor symptoms | No effect | Poor response, worsens hallucinations |
Treatment and Management
There is no cure for Parkinson’s disease dementia, but treatment focuses on symptom management and quality of life improvement.
Pharmacological Treatments
- Cholinesterase Inhibitors: Rivastigmine is FDA-approved for PDD and helps improve cognitive function.
- Dopaminergic Medications: Levodopa is used for motor symptoms but can exacerbate hallucinations.
- Atypical Antipsychotics: Quetiapine and clozapine may help manage hallucinations without worsening motor symptoms.
Non-Pharmacological Approaches
- Cognitive Therapy: Exercises to improve memory and problem-solving skills.
- Physical Therapy: Helps maintain mobility and prevent falls.
- Dietary Adjustments: Mediterranean and antioxidant-rich diets may support brain health.
- Caregiver Support: Education and respite care for family members.
The Progression of dementia associated with parkinson’s disease
The progression of PDD varies from person to person, but it generally follows a predictable course.
Coping Strategies for Patients and Caregivers
- Structured Routines: Establishing a daily schedule helps reduce confusion.
- Home Safety Modifications: Installing grab bars, removing trip hazards, and ensuring proper lighting.
- Emotional Support: Counseling and support groups for both patients and caregivers.
- Future Planning: Legal and financial planning, including advance directives and power of attorney.