Autologous bone marrow transplantation (ABMT) is a critical therapeutic approach for various hematologic malignancies, notably multiple myeloma. Despite advancements, challenges such as delays and failures in the transplantation process persist, impacting patient outcomes. This article delves into the causes, preventive measures, and implications of these challenges.
Causes of Delays in Autologous Bone Marrow Transplantation
Timing of Transplantation
The optimal timing of ABMT remains a subject of debate. Studies indicate that early transplantation, typically within 12 months of diagnosis, may offer benefits in progression-free survival (PFS). Retrospective analyses reveal that patients undergoing early ABMT have a median PFS of 28 months, compared to 18 months for those with delayed transplantation. However, overall survival (OS) rates do not show significant differences between early and late transplants.
Disease Progression and Patient Condition
Delays can also result from disease progression or the patient’s health status. Patients with aggressive disease or those who do not achieve at least a very good partial response (VGPR) prior to transplantation may experience postponements. Achieving a VGPR or better is associated with improved post-transplant outcomes.
Causes of Failure in Autologous Bone Marrow Transplantation
Engraftment Failure
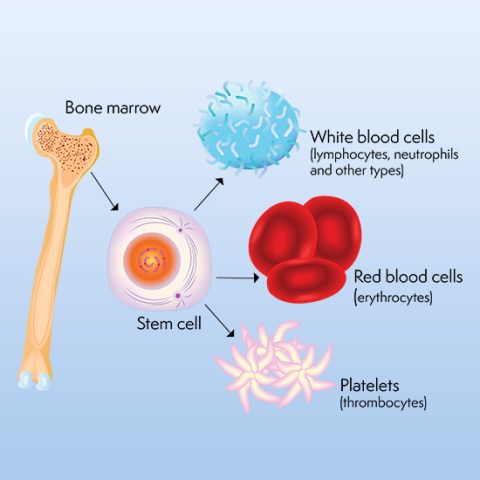
Engraftment failure, though rare in autologous transplants, occurs when the transplanted stem cells fail to establish hematopoiesis. Factors contributing to this include inadequate stem cell dose, poor stem cell quality, or damage from prior treatments. In severe cases, patients may exhibit prolonged bone marrow hypoplasia post-transplant, leading to life-threatening complications.
Graft Failure
Graft failure is an uncommon but serious complication where the bone marrow does not resume normal function post-transplant. This can lead to persistent cytopenias and increased susceptibility to infections. Causes may include contamination of the graft, inadequate stem cell numbers, or patient-related factors such as infections or immune responses.
Prevention and Management Strategies
Optimal Timing and Patient Selection
Selecting appropriate candidates and timing for ABMT is crucial. Patients achieving at least a VGPR with induction therapy are ideal candidates. Early transplantation may be beneficial, but individual patient factors must guide decisions.
Ensuring Adequate Stem Cell Collection
Adequate collection of high-quality stem cells is vital. Mobilization strategies, including the use of growth factors and, in some cases, chemotherapeutic agents, can enhance stem cell yield. Monitoring and adjusting mobilization protocols based on patient response can prevent collection issues.
Monitoring and Supportive Care
Close monitoring during the peri-transplant period allows for early detection of complications. Supportive care measures, including prophylactic antimicrobials, transfusions, and growth factor support, are essential to manage cytopenias and prevent infections.
Patient Outcomes and Prognosis
Outcomes of ABMT are influenced by various factors, including disease characteristics, patient health status, and transplant-related variables. Studies have shown that patients undergoing delayed or second ABMT for relapsed multiple myeloma had a median PFS of 19 months and a median OS of 55 months from the time of transplant. Notably, patients who underwent transplantation at first relapse had superior outcomes compared to those transplanted at later stages.