Bile acid synthesis disorders (BASDs) are a group of rare genetic conditions characterized by defects in the enzymatic pathways responsible for bile acid production. These defects impair the normal synthesis of bile acids, leading to cholestasis, fat malabsorption, and severe liver complications. Understanding the biochemical pathways and clinical implications of bile acid deficiency is crucial for accurate diagnosis and effective management.
The Role of Bile Acids in the Body
Bile acids, derived from cholesterol, play essential roles in:
- Facilitating fat digestion and absorption by emulsifying dietary lipids and promoting micelle formation.
- Maintaining cholesterol homeostasis by aiding in its excretion.
- Regulating bile flow and preventing toxic accumulation of cholesterol and metabolic waste.
The primary bile acids synthesized in humans are cholic acid and chenodeoxycholic acid. Their production involves multiple enzymatic steps in hepatocytes, and disruptions in this process can lead to significant metabolic dysfunctions.
Causes of Bile Acid Synthesis Disorders
BASDs are caused by mutations in genes encoding enzymes responsible for bile acid synthesis. These mutations follow an autosomal recessive inheritance pattern, meaning both copies of the gene must be defective for the disorder to manifest.
The most common enzyme deficiencies include:
1. 3β-Hydroxy-Δ⁵-C₂₇-Steroid Oxidoreductase Deficiency
- Caused by mutations in the HSD3B7 gene.
- Impairs conversion of cholesterol precursors into primary bile acids.
- Leads to accumulation of toxic intermediates, causing liver dysfunction.
2. Δ⁴-3-Oxosteroid 5β-Reductase Deficiency
- Results from mutations in the AKR1D1 gene.
- Prevents the reduction of Δ⁴-3-oxosteroids, disrupting bile acid synthesis.
- Causes severe neonatal cholestasis and liver fibrosis.
3. Sterol 27-Hydroxylase Deficiency (Cerebrotendinous Xanthomatosis)
- Caused by CYP27A1 mutations.
- Leads to cholesterol accumulation, tendon xanthomas, and progressive neurological symptoms.
4. Oxysterol 7α-Hydroxylase Deficiency
- Due to mutations in CYP7B1.
- Disrupts alternative bile acid synthesis pathways.
- Associated with progressive liver disease and neurodegeneration.
These deficiencies result in the accumulation of atypical bile acids and their intermediates, leading to hepatotoxicity, metabolic derangements, and multi-systemic complications.
Clinical Manifestations of Bile Acid Deficiency
Symptoms of BASDs vary depending on the specific enzyme affected and the severity of bile acid deficiency. Common clinical features include:
1. Neonatal Cholestasis
- Jaundice (yellowing of the skin and eyes)
- Dark urine and pale stools
- Hepatosplenomegaly (enlarged liver and spleen)
2. Fat-Soluble Vitamin Deficiencies
- Vitamin A Deficiency: Night blindness, dry skin
- Vitamin D Deficiency: Rickets, osteoporosis
- Vitamin E Deficiency: Neuropathy, muscle weakness
- Vitamin K Deficiency: Prolonged bleeding, easy bruising
3. Growth and Developmental Delays
- Failure to thrive in infants
- Delayed puberty and poor weight gain
4. Progressive Liver Disease
- Liver fibrosis
- Cirrhosis
- Hepatic failure in severe cases
5. Neurological Impairments (in some BASDs)
- Developmental delays
- Intellectual disabilities
- Seizures
Diagnosis of Bile Acid Synthesis Disorders
Accurate diagnosis requires a combination of clinical evaluation, biochemical testing, and genetic analysis:
- Biochemical Testing:
- Measurement of atypical bile acid metabolites in urine and blood using tandem mass spectrometry.
- Elevated levels of toxic bile acid precursors suggest enzyme deficiencies.
- Genetic Testing:
- Identification of pathogenic mutations in HSD3B7, AKR1D1, CYP27A1, CYP7B1, or other genes involved in bile acid synthesis.
- Liver Biopsy (in severe cases):
- Histological examination showing bile duct proliferation, fibrosis, and cholestasis.
Treatment Strategies for Bile Acid Deficiency
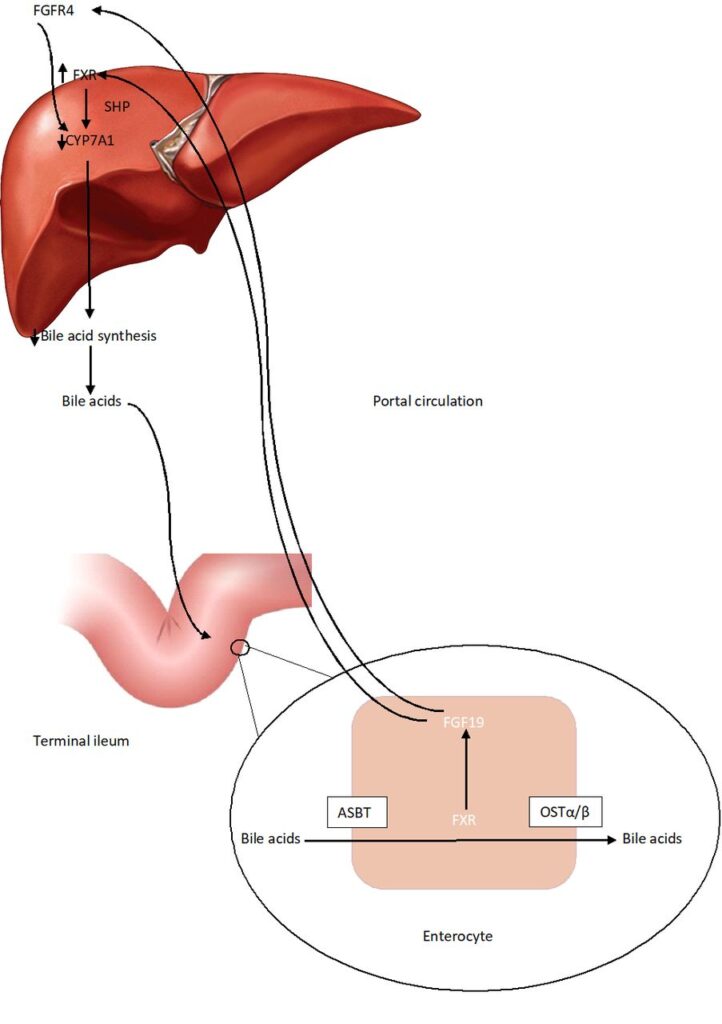
1. Bile Acid Replacement Therapy
- Cholic acid supplementation is the primary treatment for most BASDs.
- Restores normal bile acid feedback inhibition, reducing toxic precursor accumulation.
- Improves liver function and fat absorption.
2. Fat-Soluble Vitamin Supplementation
- High-dose vitamin A, D, E, and K supplementation is essential to prevent deficiencies.
3. Nutritional Support
- Medium-chain triglycerides (MCTs) in the diet can enhance fat absorption.
4. Liver Transplantation (in advanced cases)
- Considered when liver failure is present and bile acid therapy is ineffective.
Bile acid synthesis disorders result from inherited enzyme deficiencies, leading to bile acid deficiency, cholestasis, and severe metabolic complications. Early diagnosis through biochemical and genetic testing is critical to initiating bile acid replacement therapy, preventing liver damage, and improving patient outcomes. Advances in treatment, particularly cholic acid therapy, have significantly improved prognosis, though liver transplantation may be necessary in severe cases.
By understanding the molecular basis of BASDs and implementing early intervention strategies, we can mitigate disease progression and enhance quality of life for affected individuals.