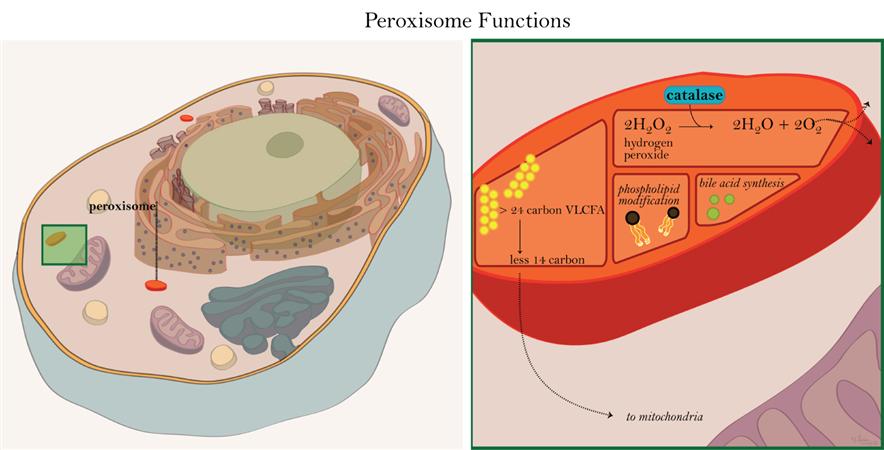
Peroxisomal disorders are a group of inherited metabolic diseases characterized by dysfunctional peroxisomes, cellular organelles essential for lipid metabolism, including bile acid synthesis. A deficiency in bile acids due to peroxisomal dysfunction disrupts cholesterol breakdown and fat digestion, leading to severe hepatic, neurological, and systemic consequences.
This article explores the mechanisms of bile acid deficiency in peroxisomal disorders, their clinical significance, and available therapeutic approaches.
Role of Peroxisomes in Bile Acid Metabolism
Bile acids are synthesized from cholesterol in the liver through a complex process requiring peroxisomal enzymes. This metabolic pathway involves:
- Cholesterol Hydroxylation – Initial modifications to convert cholesterol into bile acid precursors.
- Side-Chain Shortening in Peroxisomes – Peroxisomal β-oxidation enzymes catalyze crucial steps in bile acid synthesis.
- Conjugation and Secretion – The liver conjugates bile acids with glycine or taurine for secretion into bile.
When peroxisomes malfunction, incomplete bile acid synthesis results in the accumulation of toxic intermediates, reduced bile flow, and impaired lipid absorption.
Peroxisomal Disorders Leading to Bile Acid Deficiency
1. Zellweger Spectrum Disorders (ZSD)
A group of peroxisomal biogenesis disorders caused by mutations in PEX genes. These conditions lead to a total or partial loss of peroxisomal function, resulting in defective bile acid synthesis and accumulation of toxic intermediates.
2. D-Bifunctional Protein Deficiency
A disorder caused by mutations in the HSD17B4 gene, leading to defective β-oxidation of bile acid intermediates. This results in abnormal bile acid profiles and metabolic imbalances.
3. Alpha-Methylacyl-CoA Racemase (AMACR) Deficiency
A defect in the AMACR enzyme disrupts the conversion of bile acid precursors, leading to the accumulation of atypical bile acids, impaired fat metabolism, and neurological symptoms.
4. Acyl-CoA Oxidase Deficiency
Loss of function in the ACOX1 gene affects very-long-chain fatty acid metabolism and bile acid synthesis, contributing to progressive liver dysfunction and neurodevelopmental abnormalities.
Clinical Manifestations
Bile acid deficiency in peroxisomal disorders presents with multiple systemic symptoms, including:
- Neonatal Cholestasis – Persistent jaundice due to impaired bile flow.
- Hepatomegaly & Liver Dysfunction – Enlarged liver with progressive fibrosis or cirrhosis.
- Fat-Soluble Vitamin Deficiencies – Malabsorption of vitamins A, D, E, and K, leading to rickets, night blindness, and bleeding disorders.
- Neurological Impairments – Hypotonia, seizures, and developmental delays due to defective lipid metabolism.
- Failure to Thrive – Poor weight gain and malnutrition due to inefficient fat digestion.
Diagnostic Approaches
1. Biochemical Markers
- Elevated very-long-chain fatty acids
- Abnormal bile acid intermediates
- Decreased primary bile acids
2. Genetic Testing
- Identification of mutations in peroxisomal genes (PEX, HSD17B4, AMACR, ACOX1)
3. Liver Biopsy
- Histopathological examination to assess fibrosis and peroxisomal dysfunction
4. Imaging Studies
- Liver ultrasound and MRI to evaluate hepatic abnormalities
Treatment Strategies
1. Bile Acid Replacement Therapy
- Administration of primary bile acids (e.g., cholic acid) to restore bile acid pools and improve fat absorption.
2. Nutritional Support
- Supplementation with fat-soluble vitamins (A, D, E, K)
- Medium-chain triglycerides (MCTs) to bypass defective bile acid metabolism
3. Symptomatic Management
- Antioxidants and liver protective agents to mitigate oxidative stress
- Seizure management and physical therapy for neurological symptoms
4. Liver Transplantation
- Considered in progressive liver failure when medical therapy is ineffective.