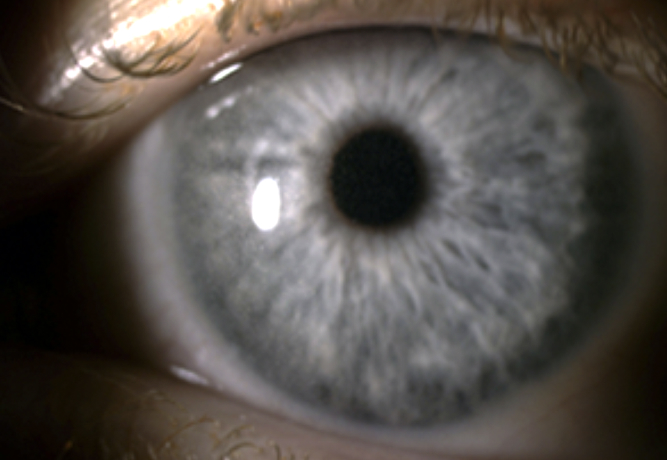
Benign cystinosis with corneal cystine crystal accumulation is a rare genetic disorder characterized by the deposition of cystine crystals in the cornea. Unlike nephropathic cystinosis, benign cystinosis does not typically affect kidney function but primarily impacts ocular health. Early recognition and appropriate management are essential for preserving vision and improving patient quality of life.
Understanding Cystinosis and Cystine Accumulation
Cystinosis is an autosomal recessive lysosomal storage disorder caused by mutations in the CTNS gene, which encodes cystinosin, a protein responsible for transporting cystine out of lysosomes. When this function is impaired, cystine accumulates within cells, leading to crystal formation in various tissues, most notably the cornea.
Clinical Manifestations
1. Corneal Cystine Crystal Deposition
- Crystalline deposits are visible in the cornea as early as infancy.
- The severity of accumulation increases with age, leading to photophobia and discomfort.
- Unlike nephropathic cystinosis, systemic involvement is rare.
2. Photophobia and Visual Disturbances
- Patients often report extreme sensitivity to light due to crystal-induced scattering.
- Visual acuity may remain unaffected in early stages but can decline with prolonged accumulation.
3. Ocular Irritation and Foreign Body Sensation
- Patients may experience persistent eye discomfort or a sensation of sand in the eyes.
- Chronic irritation can lead to secondary complications such as dry eye syndrome.
Diagnosis of Benign Cystinosis
1. Slit-Lamp Examination
- The primary diagnostic tool is a slit-lamp examination, which reveals characteristic birefringent cystine crystals within the cornea.
2. Genetic Testing
- Identification of CTNS gene mutations confirms the diagnosis.
- Differentiation from nephropathic cystinosis is essential to determine systemic involvement.
3. Cystine Measurement
- Leukocyte cystine levels may be mildly elevated but remain significantly lower than in nephropathic cystinosis.
Treatment and Management
1. Topical Cysteamine Therapy
- Mechanism: Cysteamine eye drops reduce corneal crystal accumulation by facilitating cystine breakdown.
- Dosage & Administration: Requires frequent administration (every 2 hours) for optimal effectiveness.
- Efficacy: Continuous use improves corneal clarity and alleviates photophobia.
2. Symptomatic Management
- Lubricating Eye Drops: Artificial tears help reduce irritation and improve comfort.
- Tinted Eyewear: Sunglasses with UV protection minimize photophobia.
- Corneal Transplant (Rare Cases): Indicated if corneal damage significantly impairs vision.
Prognosis and Long-Term Outlook
- Benign cystinosis remains primarily an ocular disorder with no systemic complications.
- Lifelong use of cysteamine eye drops is required to prevent progressive corneal clouding.
- Regular ophthalmologic evaluations are necessary to monitor disease progression and treatment efficacy.