Chronic myelocytic leukemia (CML) is a hematologic malignancy characterized by the presence of the Philadelphia chromosome (Ph+), which results from a reciprocal translocation between chromosomes 9 and 22. This translocation leads to the formation of the BCR-ABL1 fusion gene, a constitutively active tyrosine kinase driving leukemogenesis. The disease progresses through three distinct phases: chronic, accelerated, and blast crisis. The chronic phase is the initial stage, often asymptomatic or presenting with mild symptoms, and it is the most responsive to treatment.
Pathophysiology of Chronic Phase CML
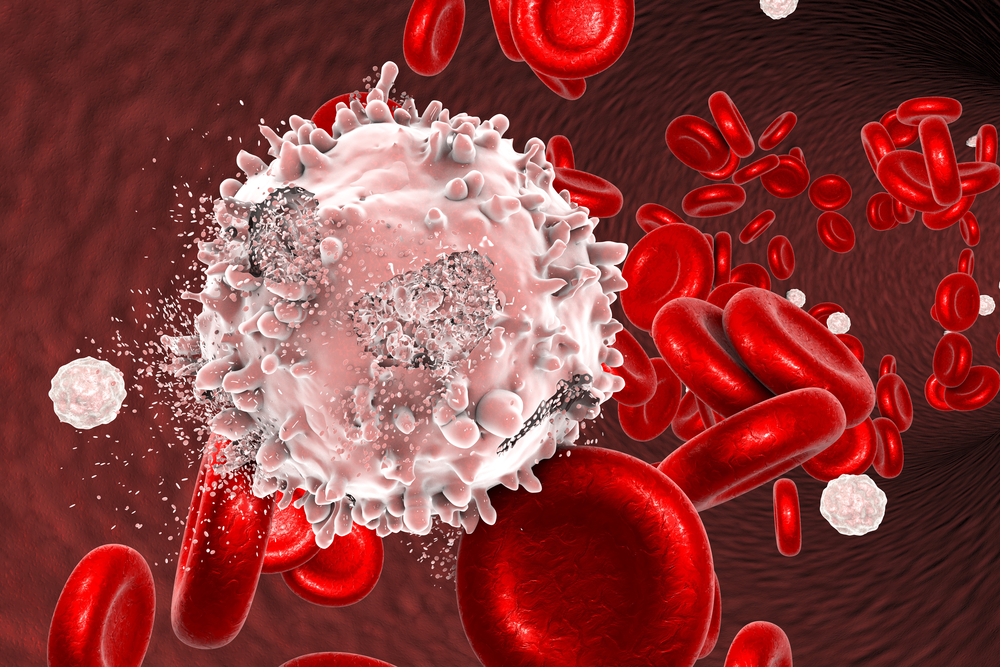
CML is primarily driven by the BCR-ABL1 fusion gene, which enhances the proliferation of myeloid cells while inhibiting apoptosis. The chronic phase is characterized by a high leukocyte count, a left-shifted myeloid series, and splenomegaly. Without intervention, CML inevitably progresses to more aggressive phases.
Clinical Presentation and Diagnosis
Symptoms
- Fatigue
- Weight loss
- Night sweats
- Abdominal discomfort (due to splenomegaly)
- Easy bruising or bleeding (less common in early stages)
Diagnostic Tests
- Complete Blood Count (CBC): Leukocytosis with a left shift
- Peripheral Blood Smear: Increased myeloid precursors
- Bone Marrow Biopsy: Hypercellular marrow with granulocytic hyperplasia
- Cytogenetic Analysis: Detection of the Philadelphia chromosome via karyotyping or fluorescence in situ hybridization (FISH)
- Molecular Testing: Quantitative PCR for BCR-ABL1 transcript levels
Treatment Strategies
Tyrosine Kinase Inhibitors (TKIs)
TKIs are the first-line treatment for chronic phase CML, targeting the BCR-ABL1 kinase and reducing leukemic cell proliferation.
| TKI | Mechanism of Action | Common Side Effects |
|---|---|---|
| Imatinib | Competitively inhibits BCR-ABL1 kinase | Edema, nausea, muscle cramps |
| Dasatinib | Inhibits multiple tyrosine kinases | Pleural effusion, cytopenias |
| Nilotinib | Selectively inhibits BCR-ABL1 | QT prolongation, metabolic abnormalities |
| Bosutinib | Dual SRC/ABL kinase inhibitor | Gastrointestinal toxicity |
| Ponatinib | Active against T315I mutation | Arterial occlusive events |
Treatment Monitoring
Response to TKIs is monitored using molecular testing to assess BCR-ABL1 transcript levels. Milestones include:
- Early Molecular Response (EMR): BCR-ABL1 ≤10% at 3 months
- Major Molecular Response (MMR): BCR-ABL1 ≤0.1% at 12 months
- Deep Molecular Response (DMR): BCR-ABL1 ≤0.01% (indicative of treatment-free remission potential)
Resistance and Treatment Adaptation
Primary resistance (failure to achieve milestones) or secondary resistance (loss of response) may necessitate:
- Mutation analysis of BCR-ABL1
- Switch to second- or third-generation TKIs
- Allogeneic stem cell transplantation for refractory cases
Prognosis and Long-Term Outcomes
Advances in TKI therapy have dramatically improved CML survival, with most patients achieving near-normal life expectancy. However, lifelong treatment adherence is crucial to prevent relapse. Research continues into treatment-free remission strategies for select patients with sustained deep molecular response.

