Cyclic neutropenia is a rare hematologic disorder characterized by recurrent fluctuations in neutrophil levels, typically occurring in 21-day cycles. During these episodes, the neutrophil count drops significantly, leaving the body vulnerable to infections. This condition, often caused by mutations in the ELANE gene, disrupts normal neutrophil production and leads to periodic immunosuppression. Understanding the pathophysiology, symptoms, diagnosis, and management of cyclic neutropenia is crucial for effective treatment and prevention of complications.
Pathophysiology and Genetic Basis
Cyclic neutropenia primarily arises due to mutations in the ELANE gene, which encodes neutrophil elastase. These mutations result in misfolded elastase proteins that trigger accelerated apoptosis in neutrophil precursors within the bone marrow. As a result, the body experiences cyclic reductions in neutrophil production, leading to predictable periods of neutropenia.
The typical cycle spans approximately 21 days, with neutrophil counts reaching their lowest point (nadir) for about 3 to 5 days before gradually recovering. This cyclic pattern of immune suppression makes individuals susceptible to recurring bacterial infections, particularly during the neutropenic phase.
Clinical Manifestations
Patients with cyclic neutropenia experience recurrent symptoms that vary in severity depending on the degree of neutropenia. The most common clinical features include:
- Recurrent Fever: A hallmark symptom, particularly during neutropenic phases, signaling underlying infections.
- Malaise and Fatigue: Generalized feelings of weakness and discomfort.
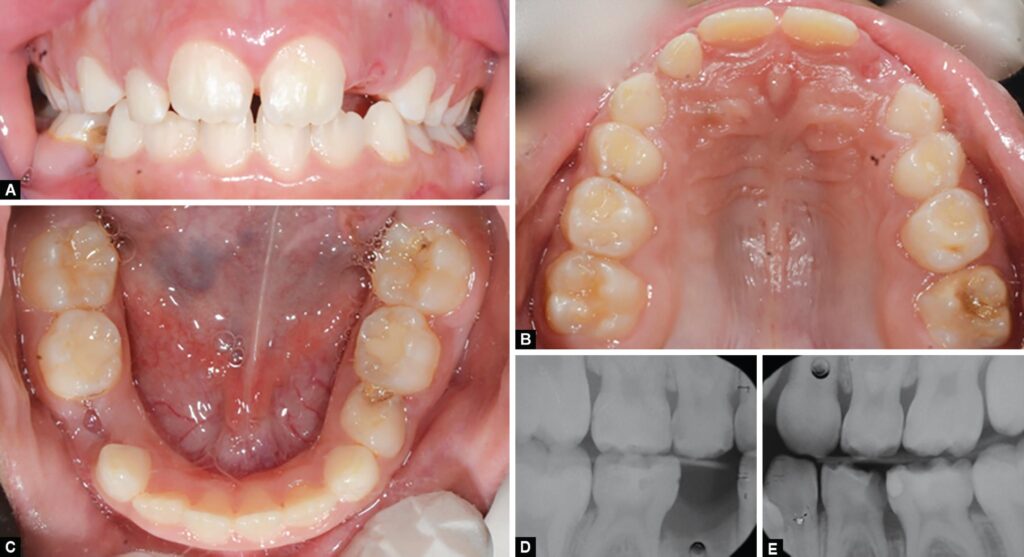
- Oral Ulcers and Gingivitis: Painful mouth sores and gum inflammation due to bacterial overgrowth.
- Pharyngitis: Sore throat caused by bacterial infections, often misdiagnosed as viral pharyngitis.
- Skin Infections: Recurrent bacterial infections such as cellulitis and abscesses.
- Respiratory Infections: Increased susceptibility to pneumonia and sinusitis during neutropenic periods.
Symptoms typically improve once neutrophil levels recover, only to return in subsequent cycles.
Diagnosis and Clinical Evaluation
Diagnosing cyclic neutropenia requires a combination of clinical history, laboratory tests, and genetic analysis. The primary diagnostic approaches include:
1. Serial Complete Blood Counts (CBCs)
A definitive diagnosis is established by monitoring neutrophil counts two to three times per week over a six-week period to identify periodic fluctuations. A pattern of cyclic neutropenia confirms the diagnosis.
2. Genetic Testing
Identifying mutations in the ELANE gene through genetic analysis helps differentiate cyclic neutropenia from other forms of neutropenia, such as severe congenital neutropenia.
3. Bone Marrow Examination
Bone marrow biopsy may reveal a decrease in neutrophil precursors, supporting the diagnosis when combined with other findings.
Management and Treatment Approaches
There is no definitive cure for cyclic neutropenia, but treatment aims to manage symptoms and prevent complications. The most effective strategies include:
1. Infection Prevention
- Maintaining excellent oral hygiene to prevent gingivitis and oral ulcers.
- Avoiding contact with sick individuals to reduce infection risks.
- Practicing meticulous wound care to prevent bacterial infections.
2. Granulocyte Colony-Stimulating Factor (G-CSF) Therapy
Filgrastim, a recombinant G-CSF, is the primary treatment for cyclic neutropenia. It stimulates neutrophil production, reduces the severity and duration of neutropenic episodes, and lowers infection risk. Regular administration can significantly improve patient outcomes.
3. Antibiotic Prophylaxis
In some cases, physicians may prescribe prophylactic antibiotics to prevent bacterial infections during neutropenic episodes. However, this approach is used cautiously to minimize the risk of antibiotic resistance.
4. Symptom Management
- Pain relief: Topical analgesics for oral ulcers.
- Antipyretics: Fever management during neutropenic episodes.
- Nutritional Support: Ensuring a balanced diet to support immune function.
Prognosis and Long-Term Outlook
With appropriate management, including G-CSF therapy and infection prevention measures, most individuals with cyclic neutropenia lead relatively normal lives. Unlike severe congenital neutropenia, cyclic neutropenia does not significantly increase the risk of leukemia. However, regular medical follow-ups are essential to monitor neutrophil trends and adjust treatment as needed.

