Acute rheumatic carditis is an inflammatory condition of the heart that arises as a complication of rheumatic fever, a post-infectious immune response to Streptococcus pyogenes. This condition primarily affects children and young adults, leading to potentially severe and chronic cardiac damage. Understanding its pathophysiology, risk factors, symptoms, and management is crucial for preventing long-term complications.
Pathophysiology of Acute Rheumatic Carditis
The disease develops due to an autoimmune response triggered by Group A Streptococcus (GAS) infections, particularly untreated or inadequately treated streptococcal pharyngitis. Molecular mimicry leads to an immune attack on cardiac tissues, resulting in inflammation of the endocardium, myocardium, and pericardium.
Risk Factors
Several factors increase susceptibility to acute rheumatic carditis, including:
- Age: Most common in children aged 5-15 years.
- Recurrent Streptococcal Infections: Frequent throat infections elevate risk.
- Genetic Predisposition: Familial clustering suggests a genetic component.
- Socioeconomic Factors: Poor access to healthcare and crowded living conditions contribute to higher incidence rates.
Clinical Symptoms
The presentation of acute rheumatic carditis includes:
- Fever and Fatigue: Systemic inflammatory response.
- Chest Pain and Palpitations: Resulting from pericarditis and myocarditis.
- Shortness of Breath: Due to valvular dysfunction and cardiac inflammation.
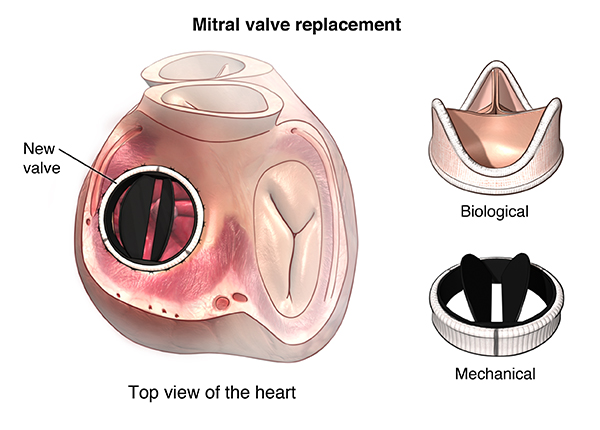
- Heart Murmurs: Indicative of mitral or aortic valve involvement.
- Joint Pain (Polyarthritis): Often precedes cardiac manifestations.
Diagnosis
Diagnosis is based on the Jones Criteria, which include:
- Major Criteria:
- Carditis (valvulitis, myocarditis, pericarditis)
- Polyarthritis
- Sydenham’s chorea
- Erythema marginatum
- Subcutaneous nodules
- Minor Criteria:
- Fever
- Elevated inflammatory markers (ESR, CRP)
- Prolonged PR interval on ECG
- Supporting Evidence:
- Positive throat culture for GAS
- Elevated antistreptolysin O (ASO) titers
Treatment Strategies
1. Antibiotic Therapy
- Penicillin or Amoxicillin: First-line treatment for streptococcal infection.
- Erythromycin or Azithromycin: Alternatives for penicillin-allergic patients.
2. Anti-inflammatory Therapy
- Aspirin or NSAIDs: Reduces fever and joint inflammation.
- Corticosteroids: Reserved for severe carditis with significant heart involvement.
3. Supportive and Long-term Management
- Bed Rest: Essential during the acute phase to reduce cardiac workload.
- Diuretics and Digoxin: Used in cases of heart failure secondary to severe carditis.
- Secondary Prophylaxis: Monthly benzathine penicillin G injections to prevent recurrence.
Prevention Strategies
- Early Treatment of Streptococcal Pharyngitis: Reduces the risk of rheumatic fever.
- Improved Hygiene and Living Conditions: Decreases transmission of GAS infections.
- Regular Follow-up: Ensures early detection and management of recurrent disease.
Prognosis and Complications
Without timely intervention, acute rheumatic carditis may lead to:
- Chronic Rheumatic Heart Disease (RHD)
- Permanent Valvular Damage (Mitral Stenosis, Aortic Regurgitation)
- Heart Failure and Arrhythmias
Early diagnosis and appropriate management significantly improve patient outcomes.
Acute rheumatic carditis is a severe inflammatory heart condition caused by an autoimmune response to streptococcal infection. Prompt recognition and treatment with antibiotics, anti-inflammatory agents, and preventive strategies are essential in minimizing complications and improving long-term cardiac health.