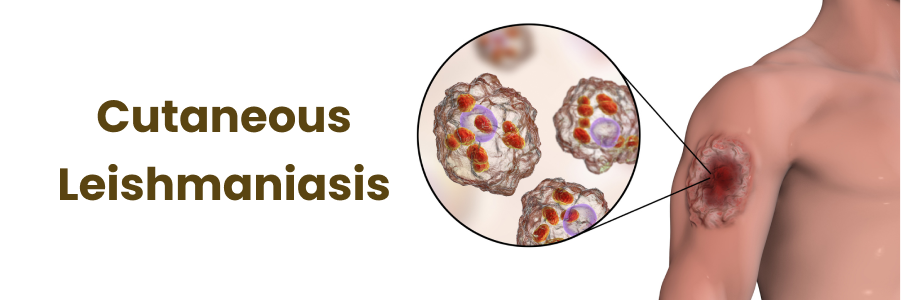
Cutaneous leishmaniasis is a parasitic skin disease caused by protozoa of the Leishmania genus, transmitted through the bite of infected female phlebotomine sandflies. It is a major health concern in tropical and subtropical regions, leading to chronic skin lesions and, in severe cases, disfigurement. Understanding its transmission, symptoms, diagnosis, and treatment is crucial for effective disease control.
Epidemiology and Geographic Distribution
Cutaneous leishmaniasis is endemic in approximately 88 countries, affecting millions worldwide. It is particularly prevalent in parts of South America, Central America, the Middle East, North Africa, and South Asia. Certain species of Leishmania have region-specific distributions, influencing disease severity and response to treatment.
Factors contributing to its spread include:
- Climate Change: Rising temperatures expand sandfly habitats.
- Deforestation: Disrupts ecological balance, increasing human-vector contact.
- Urbanization: Poor infrastructure and sanitation contribute to transmission.
- Migration and Travel: Increased human movement facilitates parasite spread.
Transmission and Life Cycle
The Leishmania parasite undergoes a complex life cycle involving both sandflies and mammalian hosts:
- An infected sandfly injects Leishmania promastigotes into human skin.
- Macrophages engulf the parasite, where it transforms into the amastigote stage.
- Amastigotes multiply, causing macrophage rupture and further infection.
- A new sandfly ingests amastigotes during a blood meal.
- Inside the sandfly, amastigotes transform into promastigotes and migrate to the proboscis, ready for the next host.
Clinical Manifestations
1. Cutaneous Leishmaniasis
- Develops as painless ulcers, nodules, or plaques.
- Lesions have raised edges with a depressed center resembling a crater.
- May heal spontaneously over months to years, leaving scars.
2. Mucocutaneous Leishmaniasis
- Affects mucosal tissues of the nose, mouth, and throat.
- Causes severe disfigurement and difficulty in breathing, eating, and speaking.
- Progresses if untreated, leading to extensive tissue destruction.
3. Diffuse Cutaneous Leishmaniasis
- Chronic form with widespread nodular skin lesions.
- Occurs in immunocompromised individuals.
- Resistant to standard treatments.
Diagnosis
Accurate diagnosis is essential for appropriate treatment. Methods include:
1. Clinical Examination
- Assessment of lesion characteristics.
- History of travel or residence in endemic regions.
2. Laboratory Tests
- Microscopy: Giemsa-stained smears to detect amastigotes.
- Culture: Growth of Leishmania in specialized media.
- PCR (Polymerase Chain Reaction): Highly sensitive and specific molecular detection.
- Serology: Limited use due to variable antibody responses.
Treatment Options
1. Systemic Therapy
- Pentavalent Antimonials (Sodium Stibogluconate, Meglumine Antimoniate): First-line drugs with known side effects such as cardiotoxicity.
- Liposomal Amphotericin B: Effective for resistant cases or severe infections.
- Miltefosine: The only oral treatment; requires caution in pregnancy.
2. Localized Therapy
- Topical Paromomycin: Effective for small, uncomplicated lesions.
- Thermotherapy: Heat application to eliminate parasites.
- Cryotherapy: Liquid nitrogen used to destroy infected tissue.
Prevention and Control
1. Personal Protection
- Use of insect repellents containing DEET or permethrin.
- Wearing protective clothing to minimize skin exposure.
- Sleeping under insecticide-treated bed nets.
2. Vector Control
- Spraying insecticides to reduce sandfly populations.
- Environmental management, such as clearing vegetation near homes.
3. Public Health Strategies
- Surveillance programs to monitor outbreaks.
- Community education on sandfly bite prevention.