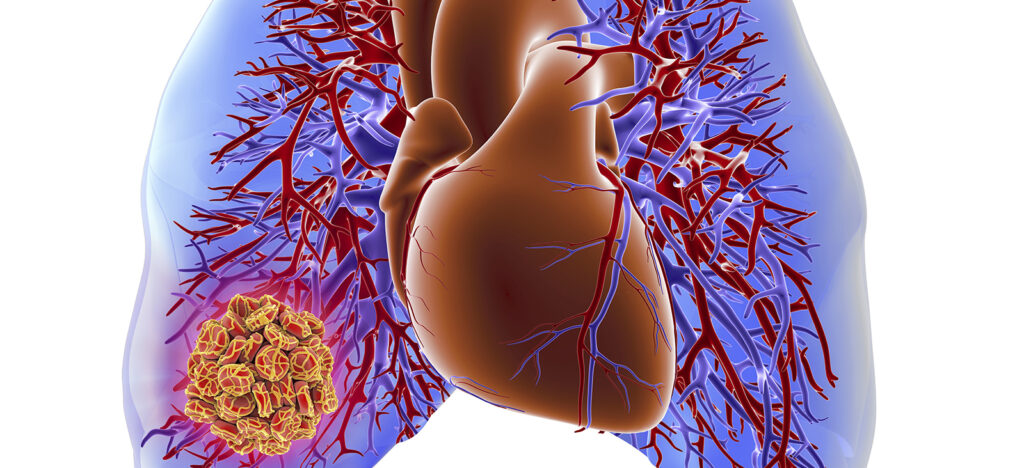
Acute pulmonary thromboembolism (APE) is a serious cardiovascular emergency caused by the sudden obstruction of pulmonary arteries due to embolic thrombi. It is a major cause of morbidity and mortality worldwide, often arising from deep vein thrombosis (DVT). Early recognition and prompt intervention are crucial for reducing fatal outcomes.
Pathophysiology of Acute Pulmonary Thromboembolism
Pulmonary embolism (PE) results from thrombus formation in the deep veins of the lower extremities, which dislodges and travels through the venous system to obstruct pulmonary circulation. This obstruction increases pulmonary vascular resistance, leading to right ventricular strain and, in severe cases, circulatory collapse.
Causes and Risk Factors
The primary cause of PE is venous thromboembolism (VTE), which includes deep vein thrombosis. Risk factors include:
- Prolonged immobility (bed rest, long flights, post-surgery recovery)
- Hypercoagulable states (genetic disorders, malignancies, pregnancy)
- Recent surgery or trauma (especially orthopedic procedures)
- Obesity and smoking
- Hormonal therapy (oral contraceptives, hormone replacement therapy)
- Chronic diseases (heart failure, cancer, inflammatory disorders)
Symptoms and Clinical Presentation
The clinical manifestations of APE vary depending on clot burden and patient condition. Common symptoms include:
- Sudden onset dyspnea (shortness of breath)
- Pleuritic chest pain (sharp pain worsened by breathing or coughing)
- Tachycardia and palpitations
- Hemoptysis (coughing up blood)
- Hypotension and syncope (indicative of massive PE)
- Cyanosis and respiratory distress (in severe cases)
Diagnosis of Pulmonary Thromboembolism
1. Clinical Assessment
- Wells Score for PE: Stratifies risk levels (low, moderate, high probability)
- D-dimer Test: Elevated levels suggest VTE but are non-specific
2. Imaging Studies
- CT Pulmonary Angiography (CTPA): Gold standard for diagnosing PE
- Ventilation-Perfusion (V/Q) Scan: Used when CTPA is contraindicated
- Echocardiography: Assesses right ventricular strain in massive PE cases
3. Additional Diagnostic Tests
- Arterial Blood Gas (ABG): Detects hypoxia and respiratory alkalosis
- Electrocardiography (ECG): May show right heart strain patterns (S1Q3T3 pattern)
- Lower Limb Doppler Ultrasound: Identifies deep vein thrombosis
Treatment Approaches
1. Anticoagulation Therapy
- First-line treatment: Low molecular weight heparin (LMWH), unfractionated heparin, or direct oral anticoagulants (DOACs) like rivaroxaban or apixaban
- Long-term management: Warfarin with INR monitoring or DOACs
2. Thrombolytic Therapy
- Indicated for massive PE with hemodynamic instability
- Alteplase (tPA): Standard thrombolytic agent
3. Surgical and Interventional Procedures
- Catheter-directed thrombolysis: Used in high-risk patients
- Pulmonary embolectomy: Considered for severe cases where thrombolysis fails
- Inferior vena cava (IVC) filter: For patients with contraindications to anticoagulation
Prevention Strategies
- Early mobilization post-surgery to prevent DVT
- Compression stockings and pneumatic devices for high-risk individuals
- Regular use of anticoagulants in patients with recurrent VTE
- Lifestyle modifications: Smoking cessation, weight management, and regular exercise
Prognosis and Complications
The prognosis of APE depends on early detection and appropriate treatment. Potential complications include:
- Chronic thromboembolic pulmonary hypertension (CTEPH)
- Right heart failure due to sustained pulmonary hypertension
- Recurrent pulmonary embolism, increasing mortality risk
Acute pulmonary thromboembolism is a medical emergency requiring swift diagnosis and treatment. Anticoagulation, thrombolytic therapy, and preventive strategies are essential in managing this life-threatening condition. Increasing awareness and early intervention can significantly improve survival rates and reduce complications.