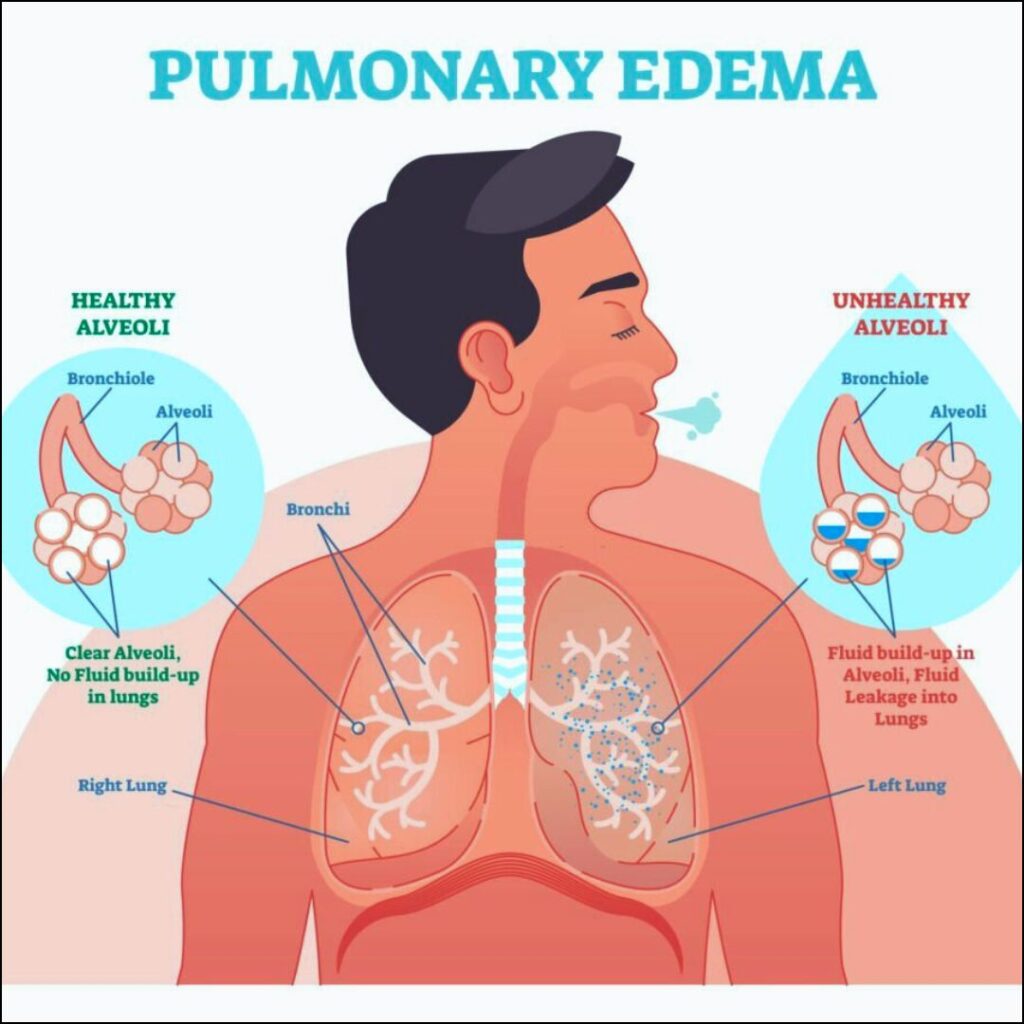
Acute pulmonary edema is a critical medical condition characterized by the rapid accumulation of fluid in the alveoli, leading to impaired gas exchange and severe respiratory distress. It is commonly associated with heart failure but may also result from non-cardiogenic factors. Prompt recognition and management are essential to prevent fatal outcomes.
Pathophysiology of Acute Pulmonary Edema
Pulmonary edema occurs due to an imbalance between hydrostatic and oncotic pressures in the pulmonary capillaries, leading to fluid leakage into the alveoli. The primary mechanisms include increased pulmonary capillary pressure (cardiogenic) or increased capillary permeability (non-cardiogenic).
Causes of Acute Pulmonary Edema
1. Cardiogenic Causes
- Left Ventricular Failure: Reduced ejection fraction leads to increased pulmonary venous pressure.
- Hypertensive Crisis: Elevated blood pressure increases cardiac workload and capillary pressure.
- Myocardial Infarction: Cardiac muscle damage results in reduced contractility and increased pulmonary congestion.
- Valvular Heart Disease: Dysfunctional valves (e.g., mitral regurgitation) cause backflow and pulmonary congestion.
2. Non-Cardiogenic Causes
- Acute Respiratory Distress Syndrome (ARDS): Inflammatory lung injury increases vascular permeability.
- Inhalation Injury: Toxic gases or smoke damage alveolar membranes.
- Sepsis: Systemic infection leads to capillary leakage.
- Neurogenic Pulmonary Edema: Increased intracranial pressure causes sympathetic overdrive, raising pulmonary pressures.
- High-Altitude Pulmonary Edema (HAPE): Hypoxia-induced vasoconstriction results in increased capillary stress.
Symptoms and Clinical Presentation
- Severe Dyspnea: Sudden onset of breathlessness, worse in a supine position.
- Cough with Frothy Sputum: Pink-tinged sputum indicates fluid leakage.
- Tachycardia and Hypertension: Common in cardiogenic cases.
- Crackles on Auscultation: Bilateral rales due to fluid accumulation.
- Cyanosis and Diaphoresis: Signs of hypoxia and distress.
Diagnosis of Acute Pulmonary Edema
- Clinical Assessment: History, symptom evaluation, and auscultation.
- Chest X-ray: Shows bilateral infiltrates and Kerley B lines.
- Echocardiography: Evaluates left ventricular function and valvular abnormalities.
- BNP (B-type Natriuretic Peptide) Levels: Elevated in cardiogenic pulmonary edema.
- Arterial Blood Gas (ABG) Analysis: Determines oxygenation and acid-base status.
Treatment and Management
1. Emergency Stabilization
- Oxygen Therapy: High-flow oxygen or non-invasive ventilation (CPAP/BiPAP) improves oxygenation.
- Intubation and Mechanical Ventilation: Required in severe cases with respiratory failure.
2. Pharmacological Treatment
- Diuretics (Furosemide): Reduces pulmonary congestion by promoting fluid excretion.
- Vasodilators (Nitroglycerin): Decreases preload and afterload, reducing cardiac stress.
- Morphine: Alleviates dyspnea and reduces sympathetic drive (use cautiously).
- Inotropes (Dobutamine, Milrinone): Improve cardiac contractility in cardiogenic cases.
3. Non-Pharmacological Interventions
- Positioning: Upright posture reduces pulmonary venous return.
- Fluid Restriction: Prevents further overload.
Prevention Strategies
- Management of Underlying Conditions: Strict control of hypertension, diabetes, and heart failure.
- Lifestyle Modifications: Salt restriction, smoking cessation, and regular exercise.
- Medication Adherence: Compliance with diuretics, antihypertensives, and heart failure therapies.
Prognosis and Complications
Prompt treatment improves outcomes, but untreated acute pulmonary edema can lead to:
- Respiratory Failure
- Multi-Organ Dysfunction
- Cardiac Arrest
Acute pulmonary edema is a life-threatening condition that requires immediate intervention. Understanding its causes, symptoms, and treatment options is crucial for effective management and prevention. Rapid diagnosis and tailored therapy significantly enhance survival rates and quality of life.