Acute Pseudomonas aeruginosa pneumonia is a life-threatening respiratory infection in individuals with cystic fibrosis (CF). This opportunistic pathogen thrives in the thick mucus of CF lungs, leading to persistent infections and rapid lung function decline. Understanding its pathogenesis, risk factors, clinical presentation, and treatment options is essential for improving patient outcomes.
Pathogenesis of Pseudomonas aeruginosa in CF Lungs
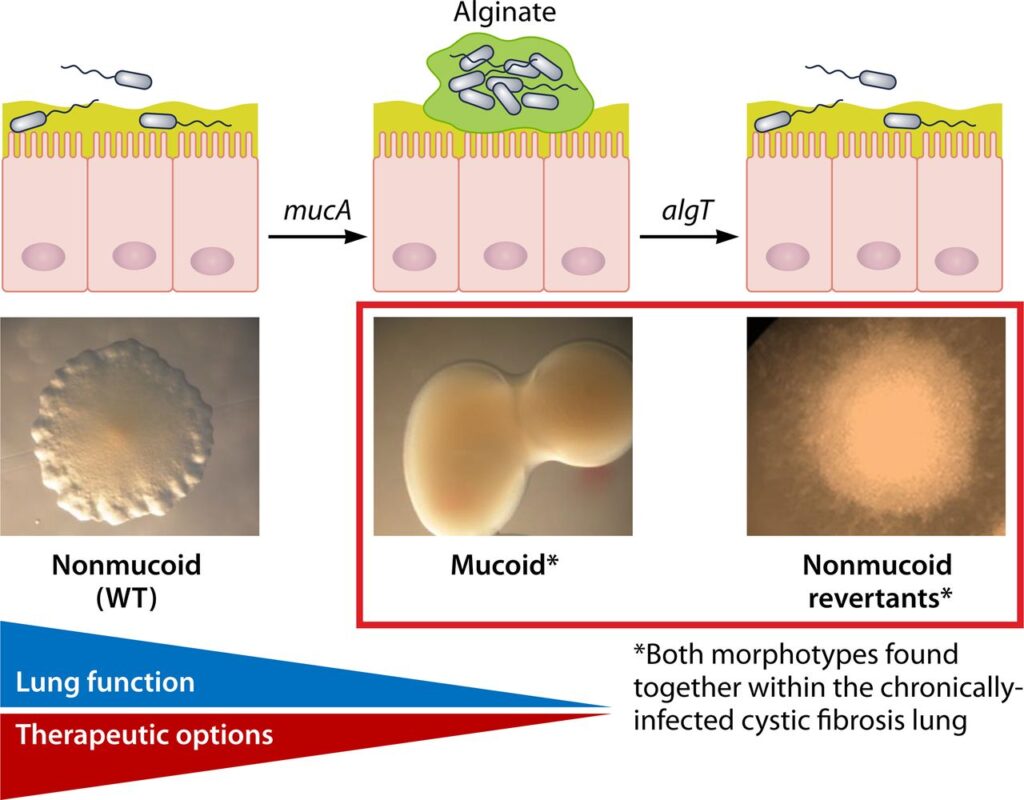
In CF patients, the genetic mutation affecting the CFTR protein results in thick, sticky mucus that creates an ideal environment for Pseudomonas aeruginosa colonization. The bacterium forms biofilms, making it highly resistant to antibiotics and immune responses.
Risk Factors for Infection
- Chronic Lung Colonization: Persistent bacterial presence in CF airways.
- Frequent Hospitalization: Exposure to resistant strains.
- Immunosuppression: Reduced immune clearance mechanisms.
- Antibiotic Use: Selects for multidrug-resistant Pseudomonas strains.
- Mechanical Ventilation: Increased risk of nosocomial infections.
Clinical Manifestations
Patients with acute Pseudomonas aeruginosa pneumonia often present with:
- Severe Cough: Persistent and productive with purulent sputum.
- Dyspnea: Progressive shortness of breath.
- Fever and Chills: Indicative of bacterial infection.
- Cyanosis: Oxygen desaturation due to respiratory compromise.
- Increased Respiratory Rate: Compensation for reduced lung function.
Diagnosis
1. Microbiological Testing
- Sputum Culture: Confirms Pseudomonas aeruginosa presence.
- Gram Staining: Identifies Gram-negative bacilli.
- Molecular PCR Testing: Detects antibiotic resistance genes.
2. Imaging Studies
- Chest X-ray: Shows infiltrates and consolidation.
- CT Scan: Provides detailed visualization of lung damage.
3. Pulmonary Function Tests (PFTs)
- FEV1 Decline: Indicates worsening airway obstruction.
Treatment Strategies
1. Antibiotic Therapy
- Beta-lactams (Piperacillin-Tazobactam, Ceftazidime, Meropenem)
- Aminoglycosides (Tobramycin, Amikacin)
- Fluoroquinolones (Ciprofloxacin, Levofloxacin)
- Nebulized Antibiotics (Tobramycin, Colistin)
2. Adjunct Therapies
- Bronchodilators: Improve airway clearance.
- Hypertonic Saline Nebulization: Facilitates mucus clearance.
- CFTR Modulators (Ivacaftor, Lumacaftor): Target underlying CF defects.
3. Oxygen and Mechanical Support
- Supplemental Oxygen: Maintains adequate oxygenation.
- Non-Invasive Ventilation (NIV): Assists in severe cases.
Prevention and Long-Term Management
- Routine Airway Clearance Therapy: Reduces bacterial load.
- Regular CF Clinic Visits: Monitors lung function.
- Strict Infection Control Practices: Prevents cross-contamination.
- Vaccination: Protects against respiratory pathogens.
Prognosis and Complications
Without prompt treatment, acute Pseudomonas aeruginosa pneumonia can lead to:
- Respiratory Failure
- Bronchiectasis Progression
- Multidrug Resistance
- Increased Mortality in CF Patients
Acute Pseudomonas aeruginosa pneumonia in cystic fibrosis patients poses a significant health burden. Effective diagnosis, timely antibiotic intervention, and ongoing CF management are crucial in preventing complications and improving patient survival.

