Cryptococcal septicemia is a rare but potentially life-threatening infection caused by the Cryptococcus species, primarily Cryptococcus neoformans and Cryptococcus gattii. This infection is predominantly associated with immunocompromised individuals, although healthy people can occasionally be affected. It is important to understand the pathophysiology, diagnostic procedures, clinical presentation, treatment options, and preventive measures associated with cryptococcal septicemia to mitigate its risk and improve outcomes.
What is Cryptococcal Septicemia?
Cryptococcal septicemia occurs when Cryptococcus fungi invade the bloodstream, leading to a systemic infection. These fungi are found in the environment, particularly in soil, bird droppings, and decaying organic material. In most cases, the infection begins in the lungs or the central nervous system, but it can disseminate to other parts of the body, including the blood, causing septicemia.
This condition is especially prevalent in individuals with weakened immune systems, such as those with HIV/AIDS, organ transplant recipients, or individuals undergoing chemotherapy. In these populations, the body’s ability to fight off fungal infections is impaired, making them more susceptible to cryptococcal infections.
Pathophysiology of Cryptococcal Septicemia
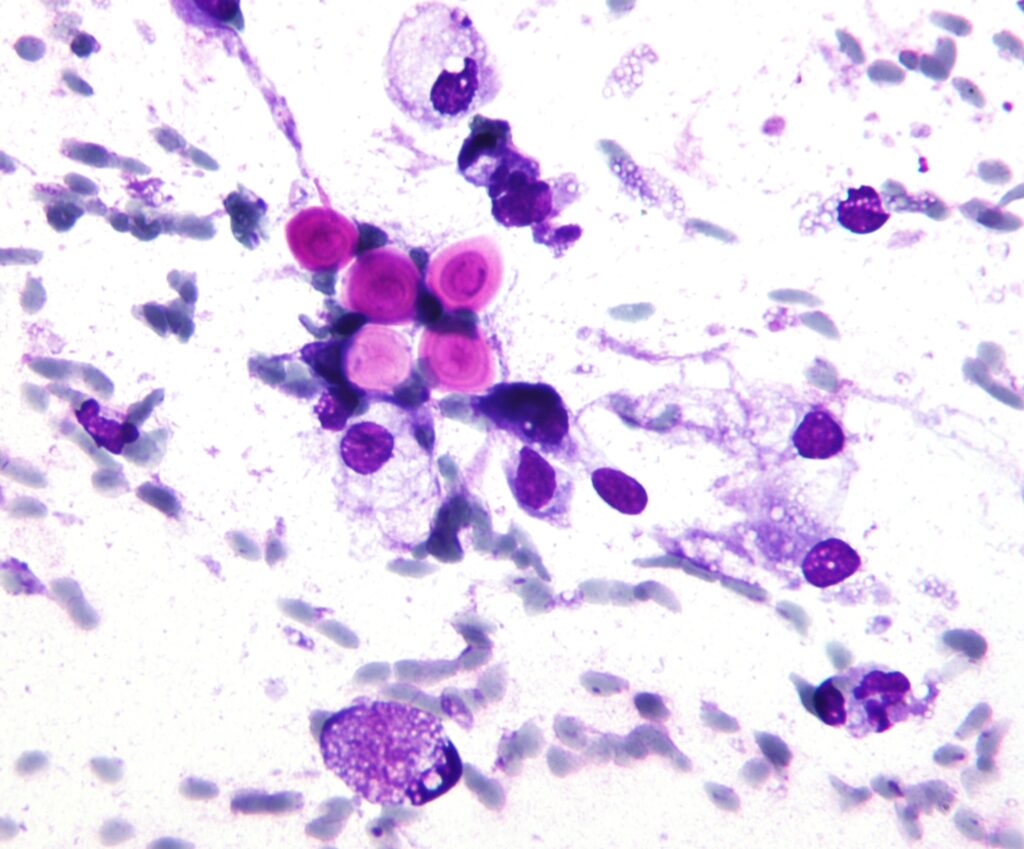
The causative agents of cryptococcal septicemia, Cryptococcus neoformans and Cryptococcus gattii, are encapsulated yeasts. The capsule helps the fungi evade the host’s immune system by inhibiting phagocytosis and impeding the action of immune cells like macrophages and neutrophils. Once the fungi enter the bloodstream, they can travel to various organs, including the lungs, brain, and skin.
Infection typically begins when a person inhales fungal spores. In healthy individuals, the immune system can control and eliminate these spores. However, in immunocompromised patients, the immune defenses are compromised, allowing the fungus to thrive and spread throughout the body.
Risk Factors
The risk factors for developing cryptococcal septicemia include:
- HIV/AIDS: Individuals with low CD4 counts are particularly at risk.
- Organ Transplantation: Immunosuppressive medications increase susceptibility.
- Cancer Treatment: Chemotherapy or radiation therapy weakens the immune system.
- Diabetes Mellitus: Chronic diabetes can contribute to a weakened immune response.
- Long-Term Steroid Use: Steroids suppress immune function.
- Chronic Lung Disease: Pre-existing lung conditions increase vulnerability.
Symptoms of Cryptococcal Septicemia
The clinical manifestations of cryptococcal septicemia can vary depending on the extent of the infection and the organs involved. Common symptoms include:
- Fever: Often one of the first signs of systemic infection.
- Fatigue and Malaise: General feelings of unwellness and fatigue.
- Weight Loss: Unexplained weight loss due to chronic infection.
- Respiratory Symptoms: Cough, shortness of breath, or chest pain, especially if the lungs are involved.
- Neurological Symptoms: Headache, confusion, and nausea, indicating potential spread to the brain and central nervous system (cryptococcal meningitis).
- Skin Lesions: In some cases, cryptococcal infections manifest as skin nodules or ulcers.
As the infection progresses, it can cause sepsis, with symptoms like hypotension, organ dysfunction, and multi-organ failure.
Diagnosis of Cryptococcal Septicemia
Timely diagnosis of cryptococcal septicemia is crucial for effective treatment. Several diagnostic tools and methods are used to identify the presence of Cryptococcus in the bloodstream:
- Blood Cultures: The gold standard for identifying bloodstream infections.
- Cryptococcal Antigen Test: This test detects the presence of fungal antigens in the blood or cerebrospinal fluid (CSF), providing rapid results.
- Polymerase Chain Reaction (PCR): PCR can detect fungal DNA and is especially useful in confirming infection in patients with negative cultures but high clinical suspicion.
- Imaging Studies: Chest X-rays or CT scans may be used to detect pulmonary involvement or complications such as abscesses or pneumonia.
- Lumbar Puncture: If cryptococcal meningitis is suspected, a lumbar puncture may be performed to examine cerebrospinal fluid for the presence of the fungus.
Treatment of Cryptococcal Septicemia
The treatment of cryptococcal septicemia involves antifungal therapy and supportive care. Early initiation of treatment significantly improves prognosis.
First-Line Antifungal Therapy
- Amphotericin B: A potent antifungal often used in combination with flucytosine for severe cases.
- Fluconazole: A triazole antifungal that is typically used for less severe infections or as step-down therapy after initial treatment with amphotericin B.
- Flucytosine: Used in combination with amphotericin B for the initial treatment of life-threatening infections.
The choice of antifungal treatment depends on the severity of the infection and the patient’s immune status. In some cases, a prolonged treatment course may be required to eradicate the infection completely.
Supportive Care
- Management of Sepsis: In septic cases, intravenous fluids, vasopressors, and other supportive measures may be necessary.
- Management of Cerebral Involvement: If cryptococcal meningitis is diagnosed, intracranial pressure may need to be monitored and controlled.
Treatment Duration
The treatment duration varies depending on the severity and location of the infection. For uncomplicated cases, antifungal therapy may last 6 to 12 weeks. However, immunocompromised patients may require lifelong maintenance therapy to prevent relapse.
Prevention of Cryptococcal Septicemia
Prevention strategies focus on reducing the risk of infection in immunocompromised individuals. These strategies include:
- Antifungal Prophylaxis: In high-risk patients, antifungal medications such as fluconazole may be prescribed as a preventive measure.
- Screening for Cryptococcal Antigen: In HIV patients with low CD4 counts, screening for cryptococcal antigens is recommended to detect asymptomatic infection early.
- Environmental Control: Reducing exposure to environments where Cryptococcus is prevalent, such as areas with bird droppings or soil contaminated with fungal spores, is recommended for immunocompromised individuals.
- Vaccination Research: Although not yet available, ongoing research into a cryptococcal vaccine may provide an additional preventive strategy in the future.
Prognosis
The prognosis for cryptococcal septicemia depends on several factors, including the patient’s immune status, the speed of diagnosis, and the adequacy of treatment. In immunocompetent individuals, the prognosis is generally favorable with proper antifungal therapy. However, in immunocompromised patients, particularly those with advanced HIV/AIDS, the infection can be fatal if not treated promptly and aggressively.