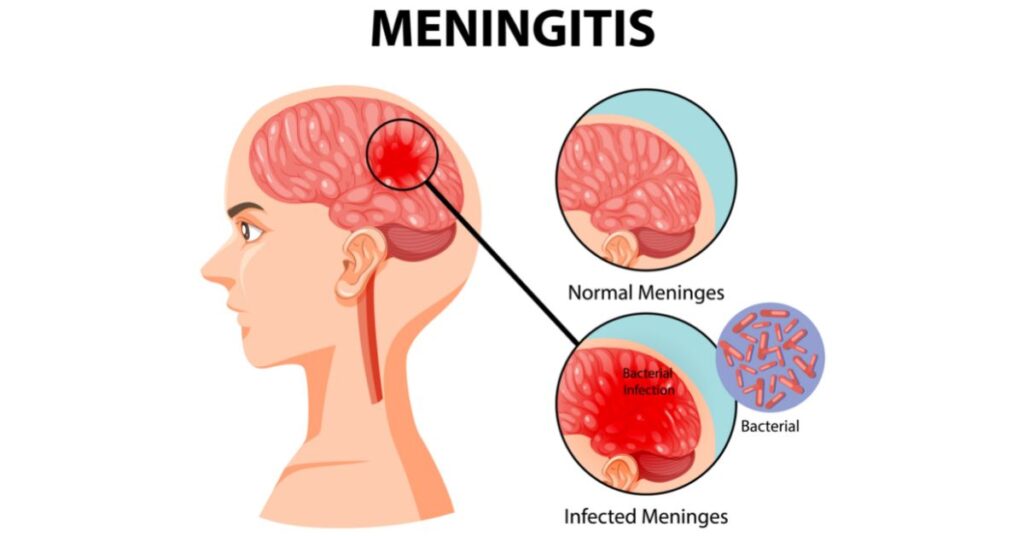
Cryptococcal meningitis is a severe fungal infection of the brain and spinal cord that primarily affects immunocompromised individuals. This disease is caused by the Cryptococcus species of fungi, which are found in the environment, particularly in bird droppings. The infection can lead to life-threatening complications if not diagnosed and treated promptly. In this detailed article, we delve into the causes, symptoms, diagnostic methods, treatment options, and preventive measures associated with cryptococcal meningitis, offering a comprehensive guide to understanding this critical condition.
What is Cryptococcal Meningitis?
Cryptococcal meningitis is an infection of the meninges, the protective membranes that surround the brain and spinal cord. The infection is caused by the Cryptococcus genus, particularly Cryptococcus neoformans and Cryptococcus gattii. These fungi can be inhaled from contaminated environments, such as soil and bird droppings, and when they enter the body, they can cause a range of neurological symptoms, most notably affecting those with weakened immune systems, such as individuals with HIV/AIDS, cancer, or those undergoing immunosuppressive treatments.
Causes of Cryptococcal Meningitis
The primary cause of cryptococcal meningitis is the inhalation of Cryptococcus spores, which are widespread in the environment. These spores enter the lungs, where they may remain dormant. However, in individuals with weakened immune systems, the spores can spread to the brain and cause meningitis. The following factors increase the risk of developing cryptococcal meningitis:
- HIV/AIDS: Individuals with HIV/AIDS are particularly susceptible due to their weakened immune system.
- Organ Transplant Recipients: Those undergoing immunosuppressive therapy to prevent organ rejection.
- Cancer Patients: Individuals with certain cancers, particularly those affecting the immune system, are at a higher risk.
- Other Conditions: Conditions like diabetes, chronic steroid use, or a history of autoimmune diseases can also increase vulnerability.
Symptoms of Cryptococcal Meningitis
Symptoms of cryptococcal meningitis can range from mild to severe, depending on the individual’s immune system status and the extent of the infection. Common symptoms include:
- Headache: Often the first and most prominent symptom, which may worsen over time.
- Fever: A common sign of infection.
- Nausea and Vomiting: These symptoms are associated with increased pressure in the brain.
- Neck Stiffness: Indicative of meningitis.
- Mental Confusion: Cognitive impairment may occur as the infection progresses.
- Seizures: In severe cases, individuals may experience seizures.
- Sensitivity to Light: Photophobia can accompany the infection.
Progression of the Disease
Without proper treatment, cryptococcal meningitis can lead to severe neurological damage, coma, and even death. Early detection and intervention are crucial to reducing the risk of these complications.
Diagnosing Cryptococcal Meningitis
Accurate and timely diagnosis is essential for the effective treatment of cryptococcal meningitis. Medical professionals rely on a variety of diagnostic tools, including:
1. Lumbar Puncture (Spinal Tap)
A lumbar puncture is the primary diagnostic test for meningitis. It involves the extraction of cerebrospinal fluid (CSF) from the spinal cord to test for the presence of Cryptococcus fungi. The CSF will often show increased pressure, white blood cells, and the presence of cryptococcal antigens.
2. Blood Tests
Blood cultures can detect Cryptococcus in the bloodstream, although this method is less sensitive than a lumbar puncture. Blood tests also help assess the overall health of the patient and identify any underlying conditions.
3. Imaging Tests
Imaging studies, such as CT scans or MRIs, can reveal swelling or inflammation in the brain. However, these tests are more useful for ruling out other causes of neurological symptoms rather than directly diagnosing cryptococcal meningitis.
4. Cryptococcal Antigen Test
This test detects cryptococcal antigens in blood, CSF, or urine samples. It is highly sensitive and commonly used for early diagnosis, especially in immunocompromised patients.
Treatment for Cryptococcal Meningitis
The treatment of cryptococcal meningitis typically involves antifungal medications. The approach depends on the severity of the infection and the patient’s immune status. The two main phases of treatment are:
1. Induction Therapy
This phase aims to rapidly reduce fungal load and includes the use of potent antifungal agents such as:
- Amphotericin B: Often administered intravenously in combination with flucytosine to target the fungal infection.
- Fluconazole: This antifungal is often used alongside amphotericin B in more mild cases or as a long-term treatment for less severe infections.
2. Consolidation and Maintenance Therapy
After the acute phase, patients may be transitioned to fluconazole for prolonged therapy. This phase can last for several months, depending on the severity of the infection and the individual’s immune response.
3. Management of Increased Intracranial Pressure
In some cases, patients may experience raised intracranial pressure due to swelling from the infection. This can be managed by draining cerebrospinal fluid or using medications to lower pressure.
Prognosis and Recovery
With appropriate treatment, the prognosis for cryptococcal meningitis can be favorable, particularly if detected early. However, the disease can be fatal in patients with severely compromised immune systems. Long-term antifungal therapy is typically required to prevent recurrence.
Preventive Measures
Preventing cryptococcal meningitis involves reducing the risk of exposure to the Cryptococcus fungus and managing underlying conditions that weaken the immune system. The following strategies can help prevent the disease:
- Antifungal Prophylaxis: In immunocompromised patients, antifungal medications such as fluconazole may be prescribed as a preventive measure.
- Environmental Precautions: Avoiding exposure to bird droppings or dust from contaminated soil, especially in areas known for higher incidences of Cryptococcus.
- Regular Monitoring: For individuals at high risk, regular blood and cerebrospinal fluid tests can help detect the infection early before symptoms appear.