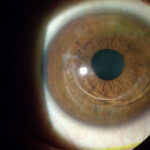
corneal edema refers to the swelling of the cornea—the transparent, dome-shaped surface that covers the front of the eye—resulting from fluid accumulation. This condition can lead to visual disturbances and discomfort. Understanding its causes, symptoms, and treatment options is essential for effective management.

Anatomy of the Cornea
The cornea comprises five distinct layers:
- Epithelium: The outermost layer serving as a barrier against dust, bacteria, and other harmful agents.
- Bowman’s Layer: A tough layer that protects the corneal stroma.
- Stroma: The thick, transparent middle layer composed of regularly arranged collagen fibers.
- Descemet’s Membrane: A thin but strong film that serves as the basement membrane for the endothelium.
- Endothelium: The innermost layer responsible for regulating fluid balance within the cornea.
The endothelium plays a pivotal role in maintaining corneal transparency by pumping excess fluid out of the stroma. Damage or dysfunction in this layer can lead to fluid accumulation and subsequent swelling.
Causes of Corneal Edema
Several factors can contribute to the development of corneal edema:
- Fuchs’ Endothelial Dystrophy: A hereditary condition characterized by the gradual loss of endothelial cells, leading to fluid buildup in the cornea.
- Eye Surgery: Procedures such as cataract surgery can sometimes damage endothelial cells, resulting in postoperative corneal edema.
- Infections: Conditions like herpes simplex keratitis can cause inflammation and damage to the corneal endothelium.
- Glaucoma: Elevated intraocular pressure can impair endothelial cell function, leading to corneal swelling.
- Contact Lens Overuse: Extended wear of contact lenses, especially overnight, can reduce oxygen supply to the cornea, causing hypoxia and subsequent edema.
- Trauma: Injury to the eye can disrupt endothelial cell integrity, resulting in fluid accumulation.
Symptoms of Corneal Edema
Individuals with corneal edema may experience:
- Blurred or Cloudy Vision: Often more pronounced upon waking and improving throughout the day.
- Halos Around Lights: Perception of rings or halos, especially in low-light conditions.
- Eye Pain or Discomfort: A sensation of grittiness or foreign body presence.
- Sensitivity to Light (Photophobia): Increased discomfort in bright environments.
- Visual Distortions: Such as seeing rainbows or glare around lights.
Diagnosis of Corneal Edema
A comprehensive eye examination is essential for diagnosing corneal edema. Ophthalmologists may employ several diagnostic tools:
- Slit-Lamp Examination: Allows detailed visualization of the cornea to assess swelling and structural changes.
- Pachymetry: Measures corneal thickness to quantify the extent of edema.
- Specular Microscopy: Evaluates endothelial cell density and morphology.
- Optical Coherence Tomography (OCT): Provides cross-sectional imaging of the cornea to assess its layers.
Treatment Options for Corneal Edema
The management of corneal edema depends on its severity and underlying cause:
- Medical Management:
- Hypertonic Saline Drops or Ointments: These solutions draw excess fluid out of the cornea, reducing swelling.
- Reducing Intraocular Pressure: Medications may be prescribed to lower eye pressure, especially if glaucoma is present.
- Anti-inflammatory Medications: Used to reduce inflammation if an underlying inflammatory condition is identified.
- Surgical Interventions:
- Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK): A partial-thickness corneal transplant that replaces the damaged endothelial layer while preserving the majority of the cornea’s structure.
- Descemet’s Membrane Endothelial Keratoplasty (DMEK): A more refined procedure that transplants only the endothelial layer and Descemet’s membrane, offering faster visual recovery and reduced rejection rates.
- Penetrating Keratoplasty (PK): A full-thickness corneal transplant reserved for cases where other treatments are ineffective.
Prevention and Management Strategies
To minimize the risk of developing corneal edema:
- Proper Contact Lens Hygiene: Adhere to recommended wear schedules, ensure lenses are cleaned appropriately, and avoid overnight wear unless specifically designed for it.
- Regular Eye Examinations: Routine check-ups can detect early signs of endothelial dysfunction or other risk factors.
- Protective Eyewear: Use appropriate eye protection during activities that pose a risk of eye injury.
- Manage Underlying Conditions: Effectively control diseases like glaucoma or diabetes that can contribute to corneal complications.
Its a condition characterized by the accumulation of fluid in the cornea, leading to visual disturbances and discomfort. Early detection and appropriate management are crucial to prevent long-term visual impairment. Individuals experiencing symptoms suggestive of corneal edema should seek prompt evaluation by an eye care professional.