Corneal ectasia following refractive surgery is a progressive condition characterized by thinning and bulging of the cornea, leading to visual impairment. While keratoconus is the most common form, ectasia can also occur as a complication following refractive surgeries such as LASIK, PRK, and SMILE. Understanding the etiology, risk factors, diagnostic methods, and treatment options is crucial for clinicians and patients considering refractive procedures.
Etiology and Pathophysiology
Post-refractive surgery ectasia is believed to result from a loss of biomechanical integrity in the cornea. Procedures like LASIK involve creating a corneal flap and ablating stromal tissue to reshape the cornea. This alteration can weaken the corneal structure, especially if pre-existing conditions or surgical parameters compromise its stability. The reduction in corneal thickness and disruption of stromal architecture may lead to progressive corneal steepening and thinning, manifesting as ectasia.
Risk Factors
Identifying patients at risk for developing corneal ectasia post-surgery is essential. Key risk factors include:
- Abnormal Preoperative Topography: Irregularities such as keratoconus, pellucid marginal degeneration, or forme fruste keratoconus increase the risk.
- Low Residual Stromal Bed (RSB) Thickness: An RSB of less than 300 microns has been correlated with an increased risk of ectasia.
- Young Age: Younger patients may have a higher susceptibility due to the potential for undiagnosed corneal instability.
- Low Preoperative Corneal Thickness: Thinner corneas are more vulnerable to biomechanical failure post-surgery.
- High Myopia: Patients with high myopic corrections may require more extensive stromal ablation, increasing the risk.
The Ectasia Risk Score System (ERSS) has been developed to assess these factors collectively, aiding in preoperative risk stratification.
Diagnostic Methods
Early detection of corneal ectasia is vital for effective management. Diagnostic approaches include:
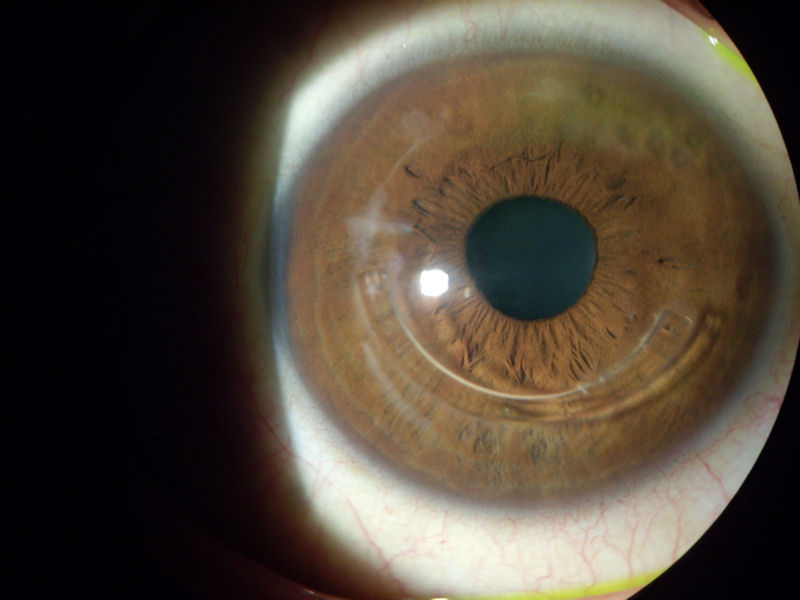
- Corneal Topography: Assesses the anterior corneal surface for irregularities and asymmetry.
- Corneal Tomography: Provides a three-dimensional view of the cornea, evaluating both anterior and posterior surfaces, as well as corneal thickness distribution.
- Pachymetry: Measures corneal thickness to identify thinning areas indicative of ectasia.
- Biomechanical Assessments: Devices like the Ocular Response Analyzer measure corneal hysteresis and resistance, offering insights into corneal stability.
Clinical Presentation
Patients with post-refractive surgery ectasia may present with:
- Progressive Myopia and Astigmatism: Increasing refractive errors leading to blurred vision.
- Decreased Uncorrected Visual Acuity (UCVA): Worsening vision without corrective lenses.
- Reduced Best-Corrected Visual Acuity (BCVA): Even with optimal correction, vision may decline.
- Glare and Halos: Patients may report visual disturbances, especially under low-light conditions.
Treatment Options
Management strategies for corneal ectasia focus on halting progression and improving visual function:
- Contact Lenses: Rigid gas permeable (RGP) lenses or scleral lenses can provide visual rehabilitation by masking corneal irregularities.
- Intracorneal Ring Segments (ICRS): Implantation of ring segments can flatten the central cornea and improve contact lens tolerance.
- Corneal Collagen Cross-Linking (CXL): A minimally invasive procedure that strengthens corneal collagen fibers, stabilizing the cornea and halting ectatic progression.
- Combination Treatments: Combining CXL with ICRS or photorefractive keratectomy (PRK) may offer synergistic benefits.
- Keratoplasty: In advanced cases, corneal transplantation, such as deep anterior lamellar keratoplasty (DALK) or penetrating keratoplasty (PKP), may be necessary.
Prevention Strategies
Preventing corneal ectasia involves meticulous preoperative assessment:
- Comprehensive Screening: Utilize advanced imaging modalities to detect subtle corneal abnormalities.
- Risk Stratification: Apply tools like the ERSS to identify high-risk patients.
- Patient Counseling: Discuss potential risks with patients, especially those with identifiable risk factors, and consider alternative refractive procedures when appropriate.