Acinetobacter pneumonia is a serious and often overlooked bacterial infection that affects the lungs, leading to significant respiratory complications. It is caused by Acinetobacter species, which are opportunistic pathogens capable of causing infections in hospitalized and immunocompromised individuals. This article provides a comprehensive overview of Acinetobacter pneumonia, exploring its causes, symptoms, diagnosis, treatment options, and prevention strategies.
What is Acinetobacter Pneumonia?
Acinetobacter pneumonia refers to a lung infection caused by the Acinetobacter bacteria. These bacteria are typically found in the environment, including soil and water, but can also be part of the normal flora of the skin and respiratory tract in some individuals. When these bacteria enter the lungs, particularly in vulnerable patients, they can cause a severe and sometimes life-threatening infection.
Acinetobacter pneumonia is most commonly encountered in hospital settings, especially in patients who are critically ill or have undergone invasive procedures. The infection is particularly concerning due to the bacteria’s resistance to multiple antibiotics, making treatment more challenging.
Causes of Acinetobacter Pneumonia
The primary cause of Acinetobacter pneumonia is infection with Acinetobacter species, with Acinetobacter baumannii being the most common pathogen. This bacterium is known for its ability to survive on surfaces for long periods, contributing to its transmission in healthcare environments. Common routes of infection include:
- Nosocomial Infections: Acinetobacter pneumonia is often acquired in healthcare settings, especially in intensive care units (ICUs), through ventilators or other medical devices.
- Direct Contact: The bacteria can spread through direct contact with contaminated surfaces or objects in the hospital.
- Invasive Procedures: Patients undergoing surgery or those with indwelling devices such as catheters and central lines are at higher risk of developing Acinetobacter pneumonia.
- Weakened Immune System: Immunocompromised individuals, such as those with cancer, diabetes, or HIV, are more susceptible to infection.
Symptoms of Acinetobacter Pneumonia
The symptoms of Acinetobacter pneumonia are similar to those of other forms of bacterial pneumonia. However, the severity of the symptoms can vary depending on the individual’s overall health and the extent of the infection. Common symptoms include:
- Fever: A high fever is often present, signaling the body’s response to the infection.
- Cough: A persistent cough, often producing mucus or phlegm, is common in individuals with pneumonia.
- Shortness of Breath: Difficulty breathing and feeling winded, even during normal activities, can occur.
- Chest Pain: Some patients experience pain in the chest, especially when coughing or breathing deeply.
- Fatigue: Due to the body fighting the infection, individuals often feel unusually tired or weak.
- Confusion: In severe cases, particularly in older adults or those with weakened immune systems, confusion or changes in mental status may occur.
Risk Factors for Acinetobacter Pneumonia
Several factors increase the risk of developing Acinetobacter pneumonia, particularly in hospitalized patients. These include:
- Prolonged Ventilator Use: Ventilator-associated pneumonia (VAP) is a common complication in patients on mechanical ventilation, where Acinetobacter bacteria can infect the lungs.
- Immunocompromised State: Patients with weakened immune systems, such as those undergoing chemotherapy or organ transplantation, are at a higher risk.
- Chronic Lung Diseases: Conditions like chronic obstructive pulmonary disease (COPD) or cystic fibrosis make individuals more susceptible to infections like Acinetobacter pneumonia.
- Previous Antibiotic Use: Overuse or misuse of antibiotics can lead to antibiotic resistance, which makes it easier for Acinetobacter to thrive.
- Severe Trauma or Surgery: Patients recovering from major surgery or trauma are more prone to infections like Acinetobacter pneumonia.
Diagnosis of Acinetobacter Pneumonia
Accurate and early diagnosis of Acinetobacter pneumonia is crucial for effective treatment. The diagnostic process typically involves a combination of clinical evaluation, imaging tests, and microbiological analysis.
1. Clinical Evaluation
The healthcare provider will assess the patient’s symptoms, medical history, and risk factors. The physical examination may reveal signs of respiratory distress, such as increased heart rate, abnormal lung sounds, or decreased oxygen levels.
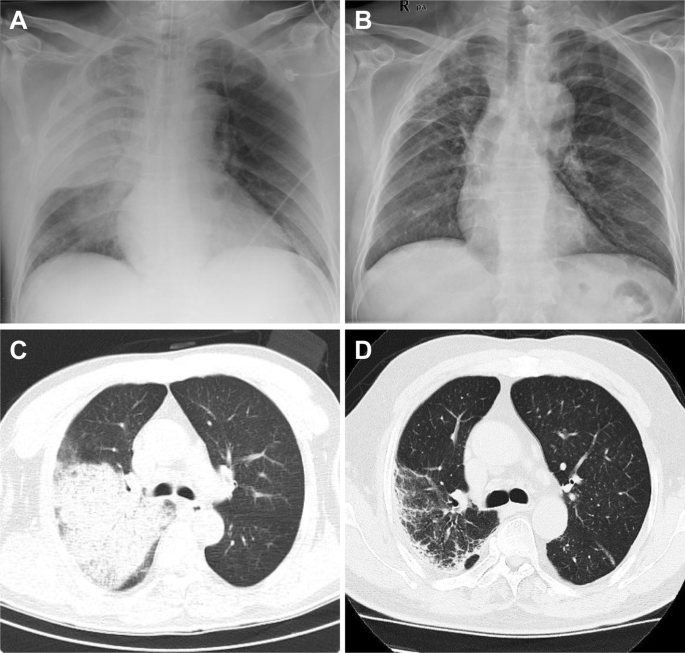
2. Chest X-Ray or CT Scan
Imaging tests are used to examine the lungs for signs of infection, including consolidation or fluid accumulation. A chest X-ray is the most common imaging method, although a CT scan may be ordered for more detailed evaluation.
3. Microbiological Testing
- Sputum Culture: A sample of sputum (mucus from the respiratory tract) is cultured in a laboratory to identify the presence of Acinetobacter and determine its antibiotic resistance profile.
- Blood Culture: In severe cases where the infection has spread to the bloodstream, a blood culture may be necessary.
- Bronchoscopy: In some cases, a bronchoscopy may be performed to collect samples directly from the lungs to confirm the diagnosis.
Treatment of Acinetobacter Pneumonia
Effective treatment of Acinetobacter pneumonia requires a tailored approach based on the severity of the infection and the specific resistance profile of the bacteria. Due to the increasing antibiotic resistance of Acinetobacter, treatment options can be limited.
1. Antibiotic Therapy
The mainstay of treatment for Acinetobacter pneumonia is antibiotic therapy. Given the bacterium’s resistance to many common antibiotics, broad-spectrum antibiotics such as carbapenems or aminoglycosides may be initially prescribed. In some cases, more specialized antibiotics, such as polymyxins or tigecycline, may be needed.
2. Combination Therapy
In severe cases, a combination of antibiotics may be used to improve efficacy and prevent the bacteria from developing resistance. The specific combination depends on the susceptibility of the bacteria as determined through culture and sensitivity testing.
3. Supportive Care
Patients with severe pneumonia may require mechanical ventilation to support breathing. Other supportive measures may include oxygen therapy, fluid management, and anti-inflammatory medications to reduce lung inflammation.
4. Surgical Intervention
In rare cases, surgical drainage may be required if there is a significant accumulation of fluid or abscess formation in the lungs.
Prevention of Acinetobacter Pneumonia
Preventing Acinetobacter pneumonia, particularly in healthcare settings, is essential for reducing the incidence of this potentially life-threatening infection. Effective prevention strategies include:
- Hand Hygiene: Proper handwashing and use of hand sanitizers by healthcare workers and patients can significantly reduce the spread of Acinetobacter.
- Infection Control Protocols: Strict infection control measures, such as isolating infected patients and using appropriate personal protective equipment (PPE), help prevent transmission.
- Antibiotic Stewardship: Limiting unnecessary antibiotic use reduces the risk of antibiotic resistance, making it harder for Acinetobacter and other bacteria to thrive.
- Proper Ventilator Care: Regular maintenance and disinfection of mechanical ventilators are crucial to reduce the risk of ventilator-associated pneumonia (VAP).
- Vaccination: While there is no specific vaccine for Acinetobacter pneumonia, vaccines for other respiratory pathogens, such as the flu and pneumococcus, can help reduce the overall risk of pneumonia.
Acinetobacter pneumonia is a serious infection that poses significant challenges in hospital settings, especially among vulnerable populations. Early detection, appropriate antibiotic treatment, and stringent infection control measures are key to managing this infection effectively. By understanding the causes, symptoms, diagnosis, treatment, and prevention strategies, healthcare providers can better prevent and treat this dangerous bacterial infection, ultimately improving patient outcomes.