Congenital toxoplasmosis is a significant public health concern and a critical topic for understanding the transmission of the parasitic infection Toxoplasma gondii from mother to child during pregnancy. This condition can have severe consequences for the newborn, causing a variety of complications if not promptly detected and treated. In this article, we will delve into the various aspects of congenital toxoplasmosis, providing in-depth information on its causes, symptoms, diagnosis, treatment, and prevention strategies.
What Is Congenital Toxoplasmosis?
Congenital toxoplasmosis occurs when a pregnant woman becomes infected with the Toxoplasma gondii parasite and transmits it to her unborn child. The infection can be passed from the mother to the fetus through the placenta, especially if the woman is first infected during pregnancy. The severity of the infection and its effects on the newborn vary depending on the timing of the infection during gestation and whether the mother receives appropriate treatment.
The Role of Toxoplasma gondii in Congenital Infection
Toxoplasma gondii is an obligate intracellular parasite that can infect a wide range of warm-blooded animals, including humans. Cats are the primary hosts of Toxoplasma and excrete oocysts in their feces, which can contaminate the environment, water, soil, or food. Humans can become infected by handling contaminated soil, ingesting undercooked meat, or drinking contaminated water.
When a woman acquires a Toxoplasma infection for the first time during pregnancy, the parasite can pass through the placenta to the fetus, causing congenital toxoplasmosis. Infections acquired before pregnancy are unlikely to lead to congenital transmission, as the immune system usually controls the infection.
Symptoms of Congenital Toxoplasmosis
The symptoms of congenital toxoplasmosis vary depending on the severity of the infection and the timing of the transmission. Some newborns with congenital toxoplasmosis may appear healthy at birth but develop long-term neurological and ocular problems. In other cases, the infection can cause severe complications at birth.
Early Symptoms in Newborns
At birth, babies affected by congenital toxoplasmosis may exhibit symptoms such as:
- Microcephaly (small head size)
- Jaundice
- Rash (often in the form of red or purple spots on the skin)
- Hepatosplenomegaly (enlarged liver and spleen)
- Severe eye damage (leading to visual impairment)
Long-term Complications
Even if the newborn appears healthy initially, congenital toxoplasmosis can lead to severe developmental and neurological problems later in life, including:
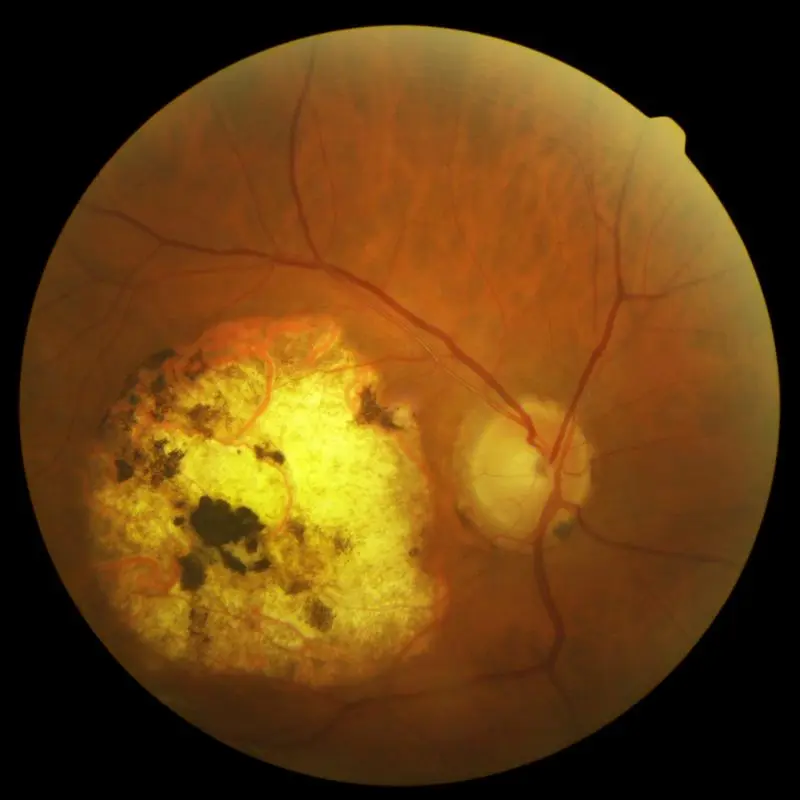
- Chorioretinitis (inflammation of the retina, leading to visual impairment)
- Cognitive disabilities
- Seizures
- Hearing loss
Asymptomatic Cases
In some instances, congenital toxoplasmosis can remain asymptomatic at birth, with symptoms developing only later in life. This is why early detection and monitoring are essential for babies born to mothers who may have contracted the infection during pregnancy.
Diagnosis of Congenital Toxoplasmosis
Early diagnosis is critical for preventing severe complications of congenital toxoplasmosis. Healthcare providers rely on a combination of prenatal screening, laboratory tests, and postnatal evaluations to diagnose the condition.
Prenatal Diagnosis
During pregnancy, women can undergo screening for Toxoplasma infection, particularly if they have risk factors, such as exposure to cats, undercooked meat, or contaminated soil. The following tests may be used:
- Serological tests: These detect antibodies indicating a recent or past infection.
- Polymerase chain reaction (PCR): PCR can identify Toxoplasma DNA in amniotic fluid, helping confirm an infection in the fetus.
Postnatal Diagnosis
After birth, a definitive diagnosis of congenital toxoplasmosis is made through:
- PCR testing of the newborn’s blood, urine, or other bodily fluids to detect Toxoplasma DNA.
- Serological testing for specific antibodies, such as IgM and IgG, which indicate an active or past infection.
In some cases, imaging tests like cranial ultrasound or magnetic resonance imaging (MRI) may be used to assess potential damage to the brain or other organs.
Treatment of Congenital Toxoplasmosis
Early treatment of congenital toxoplasmosis can reduce the risk of severe outcomes for the baby. The primary goal is to eliminate the parasite and prevent long-term complications, especially in cases where the infection is diagnosed early.
Antimicrobial Therapy
The standard treatment for congenital toxoplasmosis typically involves a combination of antimicrobial drugs, including:
- Pyrimethamine: A drug that inhibits Toxoplasma replication.
- Sulfadiazine: An antibiotic that works in synergy with pyrimethamine to prevent the parasite from reproducing.
- Leucovorin: This is given alongside pyrimethamine to reduce the risk of bone marrow suppression, a potential side effect of the drug.
Treatment is usually started as soon as the diagnosis is confirmed and can continue for several months to prevent relapse. Regular monitoring is necessary to adjust treatment and evaluate the baby’s response.
Treatment During Pregnancy
If a pregnant woman is diagnosed with Toxoplasma infection, treatment may also be initiated to reduce the risk of transmission to the fetus. Medications such as spiramycin or sulfadiazine may be used, depending on the timing of the infection and the severity of the case.
Prevention of Congenital Toxoplasmosis
Preventing congenital toxoplasmosis involves both reducing the risk of primary infection during pregnancy and providing early treatment when necessary. Key preventive measures include:
- Avoiding raw or undercooked meat: Pregnant women should avoid consuming meat that may harbor Toxoplasma cysts.
- Proper food handling: Thoroughly washing fruits, vegetables, and utensils used for preparing food to avoid contamination.
- Hygiene practices: Washing hands thoroughly after handling raw meat, soil, or cat litter to prevent infection.
- Cat management: Pregnant women should delegate cat litter box cleaning to others or wear gloves if they must handle it.
- Regular prenatal screening: Women at high risk should undergo regular serological testing to detect Toxoplasma infection during pregnancy.
Complications and Long-Term Outlook
Without early detection and treatment, congenital toxoplasmosis can lead to severe and permanent disabilities. However, with timely medical intervention, many children can lead relatively healthy lives, especially if the infection is diagnosed and treated early. Some children may require long-term care to manage vision problems, cognitive delays, or other complications associated with the infection.

