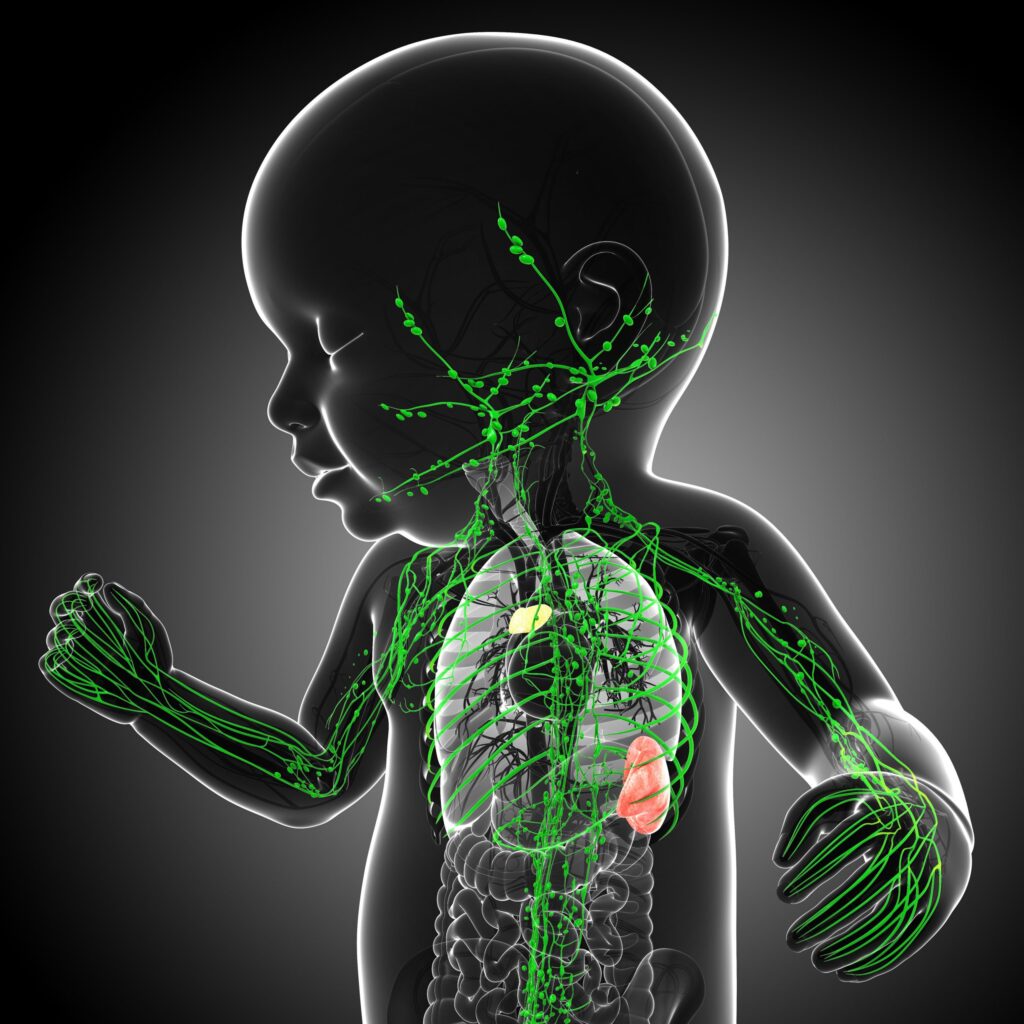
congenital athymia is a rare and life-threatening immunodeficiency disorder characterized by the absence of a functional thymus at birth. The thymus is essential for the development and maturation of T cells, which play a crucial role in adaptive immunity. Without a functioning thymus, affected individuals are highly susceptible to recurrent infections, immune dysregulation, and life-threatening complications. Early diagnosis and intervention are critical to improving outcomes in affected individuals.
Etiology and Genetic Causes
Congenital athymia arises due to genetic mutations or chromosomal abnormalities that impair thymic development. Some of the most common causes include:
FOXN1 Deficiency
Mutations in the FOXN1 gene prevent the proper development of thymic epithelial cells, leading to the absence of T-cell maturation.
22q11.2 Deletion Syndrome (DiGeorge Syndrome)
A microdeletion on chromosome 22 disrupts the TBX1 gene, which is essential for thymic organogenesis. This leads to thymic aplasia or hypoplasia, causing profound immunodeficiency.
CHARGE Syndrome
Mutations in the CHD7 gene, which plays a role in multiple organ developments, can lead to congenital athymia due to disrupted thymic formation.
PAX1 Mutations
PAX1 mutations affect thymic and skeletal development, resulting in a lack of thymic tissue and subsequent immune dysfunction.
These genetic abnormalities highlight the complexity of thymic development and its dependence on multiple regulatory genes.
Clinical Manifestations
The absence of a thymus results in severe T-cell immunodeficiency, leading to:
- Recurrent and Severe Infections
Affected individuals experience frequent bacterial, viral, and fungal infections due to the absence of functional T cells. - Immune Dysregulation and Autologous Graft-versus-Host Disease (GVHD)
Some patients develop skin rashes, diarrhea, and liver dysfunction due to oligoclonal T cells that cause immune dysregulation. - Autoimmune Disorders
The immune system’s inability to self-regulate leads to autoimmune conditions such as autoimmune thyroiditis and hemolytic anemia.
Due to these severe complications, congenital athymia requires immediate medical attention and appropriate interventions.
Diagnostic Approach
Early detection of congenital athymia is essential for effective management. The diagnostic process includes:
Newborn Screening
Many affected individuals are identified through newborn screening programs that detect T-cell receptor excision circles (TRECs), an indicator of T-cell production.
Flow Cytometry
Lymphocyte subset analysis reveals an absence or severe reduction of T cells while maintaining normal B-cell and Natural Killer (NK) cell counts (T^-B^+NK^+ phenotype).
Genetic Testing
Molecular analysis of FOXN1, TBX1, CHD7, and PAX1 genes confirms the underlying genetic mutation responsible for thymic aplasia.
Differentiation from severe combined immunodeficiency (SCID) is critical, as both conditions share similar immunological profiles but require distinct therapeutic approaches.
Therapeutic Interventions
Historically, congenital athymia was considered a fatal condition. However, recent advancements in treatment offer new hope.
Thymus Tissue Transplantation
Thymus transplantation is the only curative therapy for congenital athymia. It involves the transplantation of allogeneic processed thymus tissue, which supports T-cell development and immune system reconstitution. This therapy has shown promising results, with immune function restoration typically occurring within six months post-transplantation.
Supportive Care
Patients require rigorous infection prevention strategies, including prophylactic antibiotics, antifungals, and intravenous immunoglobulin (IVIG) therapy to provide passive immunity.
Prognosis and Outcomes
Without treatment, congenital athymia is fatal within the first few years of life due to overwhelming infections and immune failure. Thymus transplantation has dramatically improved survival rates, offering long-term immune reconstitution and a functional T-cell population. Early diagnosis and timely intervention remain key factors in improving prognosis.