Allogeneic hematopoietic stem cell transplantation (HSCT) stands as a pivotal therapeutic intervention for various hematologic disorders. A critical component of this procedure is the conditioning regimen administered before the infusion of donor stem cells. This article delves into the intricacies of conditioning regimens, elucidating their purposes, classifications, and the factors influencing their selection.
Objectives of Conditioning Regimens
The conditioning regimen serves multiple essential functions:
- Disease Eradication: In malignant conditions, the regimen aims to eliminate residual cancer cells, thereby reducing the risk of relapse.
- Immunosuppression: Adequate immunosuppression is necessary to prevent the recipient’s immune system from rejecting the donor stem cells.
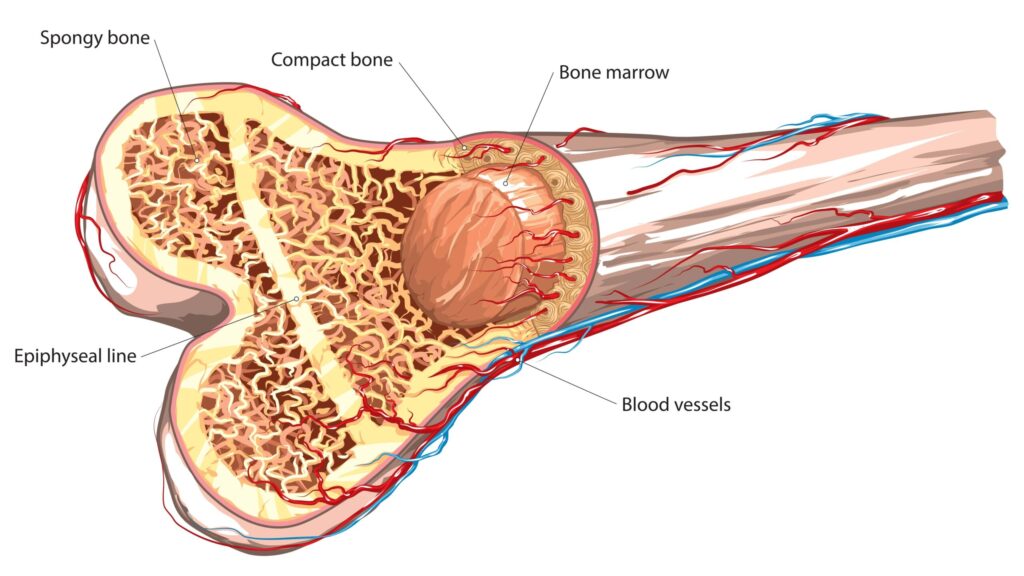
- Marrow Space Creation: By depleting the host’s bone marrow, the regimen creates space for the engraftment of donor stem cells.
Classification of Conditioning Regimens
Conditioning regimens are broadly categorized based on their intensity and components:
Myeloablative Conditioning (MAC)
MAC involves high-dose chemotherapy, often combined with total body irradiation (TBI). This approach effectively eradicates malignant cells and ensures profound immunosuppression. However, it is associated with significant toxicity, limiting its use to younger patients without substantial comorbidities.
Reduced-Intensity Conditioning (RIC)
RIC employs lower doses of chemotherapy and/or radiation, aiming to reduce toxicity while providing sufficient immunosuppression to facilitate engraftment. This regimen is particularly beneficial for older patients or those with existing comorbidities. While RIC is associated with a higher risk of disease relapse compared to MAC, it offers a more favorable safety profile for certain patient populations.
Components of Conditioning Regimens
The specific agents and modalities used in conditioning regimens vary, but commonly include:
- Chemotherapy Agents: Drugs such as cyclophosphamide, busulfan, and fludarabine are frequently utilized for their cytotoxic and immunosuppressive properties.
- Total Body Irradiation (TBI): TBI is employed to eradicate residual malignant cells and provide immunosuppression. It is particularly effective in targeting sanctuary sites that may be less accessible to chemotherapy agents.
- Immunotherapy: Agents like antithymocyte globulin (ATG) are incorporated to enhance immunosuppression and reduce the risk of graft rejection.
Factors Influencing Regimen Selection
The choice of conditioning regimen is influenced by several factors:
- Patient Age and Comorbidities: Older patients or those with significant comorbidities may not tolerate the toxicity associated with MAC, making RIC a more suitable option.
- Disease Characteristics: The type and stage of the underlying disease play a crucial role in regimen selection. For instance, aggressive malignancies may necessitate the use of MAC to achieve optimal disease control.
- Donor Source: The compatibility and source of the donor stem cells (e.g., matched sibling donor vs. unrelated donor) can influence the intensity of the conditioning regimen.
Potential Complications
While conditioning regimens are integral to the success of HSCT, they are associated with potential complications:
- Regimen-Related Toxicity: High-dose chemotherapy and radiation can lead to organ toxicity, with the gastrointestinal tract, liver, and lungs being particularly susceptible.
- Graft-Versus-Host Disease (GVHD): The immunosuppressive nature of conditioning regimens increases the risk of GVHD, a condition where donor immune cells attack the recipient’s tissues.

