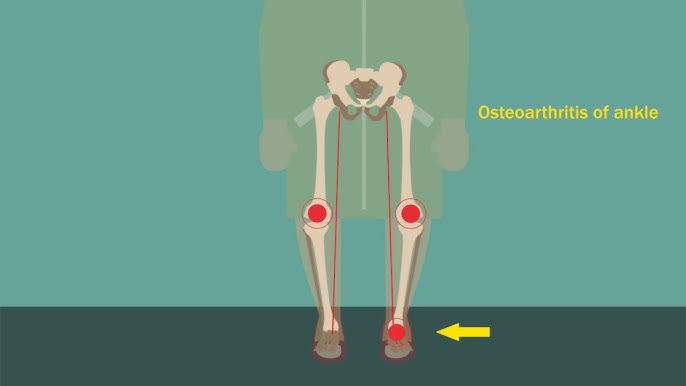
Concomitant hypertension and osteoarthritis Its a Hypertension and osteoarthritis (OA) are two of the most prevalent chronic conditions worldwide, frequently coexisting in aging populations. Their concurrence presents unique clinical challenges due to overlapping risk factors, shared pathophysiological mechanisms, and complex treatment interactions. Understanding their interplay is essential for effective disease management and improved patient outcomes.
Epidemiology of Hypertension and Osteoarthritis
Hypertension affects over a billion people globally, while OA remains the leading cause of disability in adults. Studies suggest that individuals with OA have a higher prevalence of hypertension compared to the general population, possibly due to systemic inflammation, metabolic factors, and decreased physical activity resulting from joint pain. This bidirectional relationship emphasizes the need for an integrated approach to patient care.
Shared Risk Factors
Several risk factors contribute to the concomitant presence of hypertension and OA:
- Age: Both conditions become more prevalent with advancing age due to physiological wear and decreased regenerative capacity.
- Obesity: Excess weight increases joint stress, accelerating cartilage breakdown, while also contributing to hypertension through metabolic and inflammatory pathways.
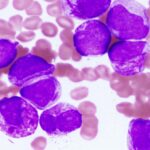
- Chronic Inflammation: Low-grade systemic inflammation plays a significant role in both conditions, exacerbating joint degeneration and vascular dysfunction.
- Sedentary Lifestyle: Reduced physical activity, often due to OA-related pain, can lead to weight gain and worsening of hypertension.
- Genetic Predisposition: Family history is a known risk factor for both conditions, indicating possible genetic contributions to their development.
Pathophysiological Mechanisms Linking Hypertension and Osteoarthritis
The coexistence of hypertension and OA is not merely coincidental. Several mechanisms explain their interconnection:
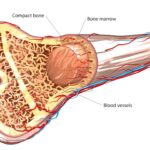
- Vascular Insufficiency: Hypertension can impair microvascular circulation, leading to subchondral bone ischemia, which contributes to cartilage degeneration in OA.
- Oxidative Stress: Increased oxidative stress is observed in both conditions, leading to cellular damage in joints and blood vessels.
- Renin-Angiotensin System (RAS) Dysregulation: Activation of RAS has been implicated in both OA and hypertension, promoting inflammation, fibrosis, and tissue remodeling.
- Sympathetic Nervous System Overactivity: Chronic stress and autonomic dysfunction can exacerbate both hypertension and joint pain.
Clinical Implications
The presence of both hypertension and OA requires careful medical management due to overlapping treatment considerations:
- Pain Management Challenges: NSAIDs, commonly used for OA pain relief, can raise blood pressure, posing risks for hypertensive patients.
- Medication Interactions: Certain antihypertensive drugs may influence joint function and pain perception.
- Cardiovascular Risks: Patients with both conditions are at an increased risk of cardiovascular complications, necessitating comprehensive monitoring.
Management Strategies
A multidisciplinary approach is crucial for managing patients with both hypertension and OA. Key strategies include:
1. Lifestyle Modifications
- Weight Management: Reducing excess body weight alleviates joint stress and improves blood pressure control.
- Exercise: Low-impact activities, such as swimming and cycling, help maintain joint function while promoting cardiovascular health.
- Dietary Adjustments: A balanced diet rich in anti-inflammatory foods can mitigate symptoms of both conditions.
2. Pharmacological Considerations
- Pain Management: Acetaminophen or topical treatments may be preferred over NSAIDs to minimize cardiovascular risks.
- Blood Pressure Control: Choosing antihypertensive medications that do not exacerbate joint pain is critical.
- Supplements: Chondroprotective agents like glucosamine and chondroitin may support joint health without affecting blood pressure.
3. Regular Monitoring and Multidisciplinary Care
- Blood Pressure Checks: Frequent monitoring is essential to adjust medications accordingly.
- Joint Health Assessment: Routine evaluations help track disease progression and optimize treatment.
- Collaboration Between Specialists: Coordinated care between rheumatologists, cardiologists, and primary care providers ensures a balanced treatment approach.