Acute osteomyelitis is a serious bacterial infection of the bone that requires prompt medical intervention to prevent complications such as bone destruction, abscess formation, and systemic infection. It commonly affects children and immunocompromised individuals but can occur at any age. Early detection and aggressive treatment are critical for preventing long-term morbidity.
Pathophysiology of Acute Osteomyelitis
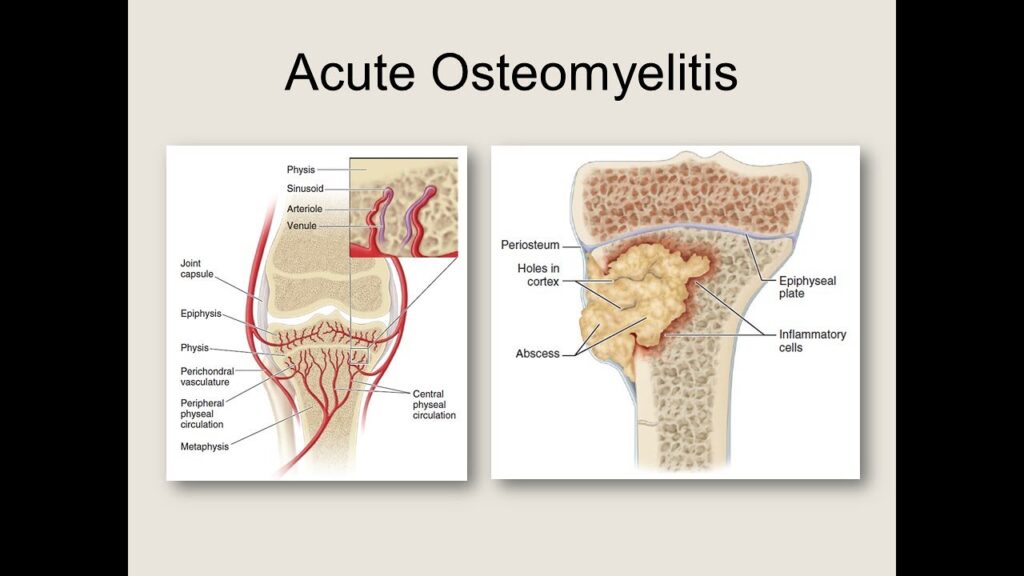
Acute osteomyelitis typically results from hematogenous spread, direct inoculation from trauma, or contiguous infection. The inflammatory response within the bone leads to necrosis, increased intraosseous pressure, and potential abscess formation.
Causes and Risk Factors
Common Causative Pathogens
- Staphylococcus aureus (most common)
- Streptococcus pyogenes
- Pseudomonas aeruginosa
- Escherichia coli (especially in neonates)
Risk Factors
- Recent bone trauma or surgery
- Diabetes mellitus
- Intravenous drug use
- Immunosuppression (e.g., chemotherapy, HIV)
- Poor circulation (e.g., peripheral vascular disease)
Clinical Presentation
Symptoms
- Sudden onset of localized bone pain
- Swelling and redness over affected area
- Fever, chills, and malaise
- Limited range of motion in adjacent joints
- Warmth and tenderness over the infected bone
Signs in Pediatric vs. Adult Populations
- Children: Often present with high fever, irritability, and refusal to use the affected limb (pseudoparalysis).
- Adults: Symptoms may be more insidious with chronic low-grade fever and localized pain.
Diagnostic Approach
Laboratory Investigations
- Complete Blood Count (CBC): Elevated white blood cell count
- C-Reactive Protein (CRP) & Erythrocyte Sedimentation Rate (ESR): Markers of inflammation
- Blood Cultures: Identifies causative organism in hematogenous cases
Imaging Studies
- X-ray: May show bone destruction in late stages
- MRI: Gold standard for early detection of bone marrow involvement
- CT Scan: Useful for assessing bone sequestra
- Bone Biopsy & Culture: Confirms the pathogen for targeted antibiotic therapy
Treatment Strategies
1. Empiric and Targeted Antibiotic Therapy
- Empiric therapy: Vancomycin + Ceftriaxone (broad coverage until cultures return)
- Pathogen-specific treatment:
- S. aureus: Nafcillin, Oxacillin, or Vancomycin (if MRSA is suspected)
- Pseudomonas: Ceftazidime or Piperacillin-Tazobactam
- E. coli: Third-generation cephalosporins
2. Surgical Management
- Debridement: Removal of necrotic bone tissue
- Drainage of Abscess: Prevents systemic spread
- Limb Salvage Procedures: Necessary in severe cases
3. Supportive Care
- Pain management with NSAIDs or opioids
- Immobilization with splints to reduce pain and prevent further damage
- Nutritional support for optimal healing
Complications
- Chronic osteomyelitis
- Septic arthritis
- Pathologic fractures
- Growth disturbances in pediatric cases
- Sepsis and multi-organ involvement
Prevention and Prognosis
Prevention
- Prompt treatment of soft tissue infections
- Sterile techniques during surgeries and wound care
- Proper management of chronic conditions like diabetes
Prognosis
With early and aggressive treatment, the prognosis of acute osteomyelitis is generally favorable. However, delayed diagnosis can lead to chronic infection and long-term disability.
Acute osteomyelitis is a medical emergency requiring timely intervention. Early diagnosis through imaging and laboratory tests, coupled with appropriate antibiotic therapy and, if necessary, surgical intervention, ensures the best possible outcome for affected patients.

