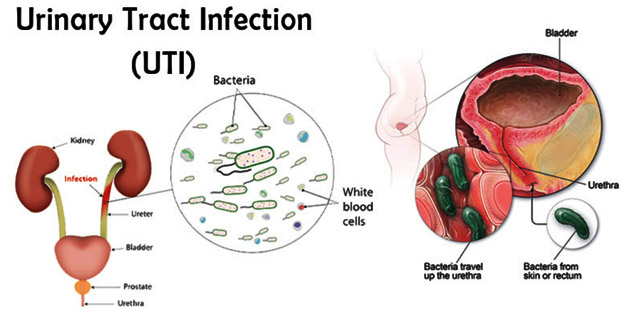
Urinary tract infections (UTIs) are among the most common bacterial infections, affecting individuals across all age groups. While many UTIs can be easily treated with antibiotics, some cases present significant challenges. Complicated urinary tract infections (cUTIs) are a subset of these infections, typically associated with factors that make them more difficult to treat or manage. One of the notable pathogens responsible for cUTIs is Acinetobacter, a versatile and opportunistic bacterium that can cause severe complications, particularly in hospital settings.
What is Acinetobacter?
Acinetobacter is a genus of gram-negative bacteria commonly found in soil, water, and on the skin of humans. While often harmless, certain species of Acinetobacter, particularly Acinetobacter baumannii, are opportunistic pathogens capable of causing a range of infections, including UTIs. Acinetobacter infections are particularly concerning in immunocompromised patients or those who have undergone invasive procedures.
What Makes a UTI Complicated?
A UTI is classified as complicated when the infection occurs in individuals with underlying health conditions or anatomical abnormalities that make the infection more difficult to treat. These infections often involve deeper parts of the urinary system, such as the kidneys or bladder, and may be associated with resistance to standard antibiotics. Complicated UTIs can lead to severe complications, including renal damage, sepsis, or even death if not adequately managed.
The Pathophysiology of Acinetobacter-Related UTIs
Acinetobacter UTIs often occur as healthcare-associated infections (HAIs), particularly in patients with long-term catheterization, recent surgeries, or those who are critically ill. The bacteria enter the urinary tract through various mechanisms, such as ascending infection from the perineum or via direct contamination from medical devices.
Once Acinetobacter gains access to the urinary tract, it adheres to the epithelial cells lining the bladder and kidneys, forming biofilms that protect the bacteria from both the host immune system and antibiotics. This biofilm formation is a key factor in the persistence of the infection and its resistance to treatment.
Risk Factors
Several risk factors contribute to the development of complicated UTIs caused by Acinetobacter:
- Hospitalization: Extended stays in hospitals, especially in intensive care units (ICUs), increase the risk due to exposure to invasive devices like catheters and ventilators.
- Immunocompromised states: Conditions such as diabetes, cancer, and immunosuppressive therapies weaken the immune system, making patients more vulnerable to infections.
- Antibiotic resistance: Acinetobacter is known for its ability to develop resistance to multiple classes of antibiotics, complicating treatment options.
Symptoms and Clinical Manifestations
The symptoms of a complicated UTI caused by Acinetobacter can be severe and may include:
- Dysuria: Painful urination
- Hematuria: Blood in the urine
- Fever: Elevated body temperature due to systemic infection
- Flank pain: Pain in the lower back or sides, indicative of kidney involvement
- Sepsis: In severe cases, Acinetobacter UTIs can lead to systemic infection, causing sepsis with symptoms such as hypotension, confusion, and organ failure.
Diagnostic Approaches to Acinetobacter UTIs
Accurate diagnosis is critical in managing complicated UTIs caused by Acinetobacter. The primary diagnostic tools include:
- Urine culture: The gold standard for identifying the causative pathogen. Cultures can reveal the presence of Acinetobacter and determine antibiotic susceptibility.
- Blood cultures: In cases of systemic infection or sepsis, blood cultures help confirm bacteremia.
- Imaging: Ultrasonography or CT scans may be used to assess for complications such as abscesses, pyelonephritis, or renal failure.
- Antibiotic susceptibility testing: Given the growing concern over antibiotic resistance, determining the specific resistance patterns of Acinetobacter is essential to guide therapy.
Treatment Strategies for Complicated UTIs Due to Acinetobacter
Treating complicated UTIs caused by Acinetobacter presents significant challenges, particularly in the face of antibiotic resistance. The therapeutic approach typically involves a combination of the following:
1. Antibiotic Therapy
Given the multi-drug-resistant nature of Acinetobacter, empirical antibiotic therapy is often initiated based on local resistance patterns, followed by targeted therapy once culture results are available. Commonly used antibiotics include:
- Carbapenems: These are the first-line treatment for most Acinetobacter infections, though resistance is becoming increasingly common.
- Colistin: A polymyxin antibiotic often reserved for multidrug-resistant strains.
- Tigecycline: Another option for resistant infections, particularly in critically ill patients.
2. Supportive Care
In severe cases, particularly those involving sepsis or renal failure, supportive care is essential. This may include intravenous fluids, vasopressors to support blood pressure, and renal replacement therapy if kidney function deteriorates.
3. Prevention and Infection Control
Preventing the spread of Acinetobacter in healthcare settings is crucial. Key measures include:
- Hand hygiene: Rigorous handwashing and the use of hand sanitizers.
- Sterile technique: Proper care and maintenance of catheters and other invasive devices.
- Isolation protocols: Patients infected with Acinetobacter should be isolated to prevent nosocomial transmission.
Antibiotic Resistance and Challenges in Treatment
The growing issue of antibiotic resistance in Acinetobacter has made treating complicated UTIs more difficult. Acinetobacter has acquired resistance to nearly all commonly used antibiotics, including beta-lactams, aminoglycosides, and fluoroquinolones. The rise of carbapenem-resistant Acinetobacter (CRAB) strains further complicates treatment, requiring the use of last-resort antibiotics like colistin or tigecycline, which are associated with higher toxicity.
As resistance continues to increase, new treatment options are desperately needed. Ongoing research into novel antibiotics, bacteriophage therapy, and alternative treatments holds promise for the future of Acinetobacter infections.

