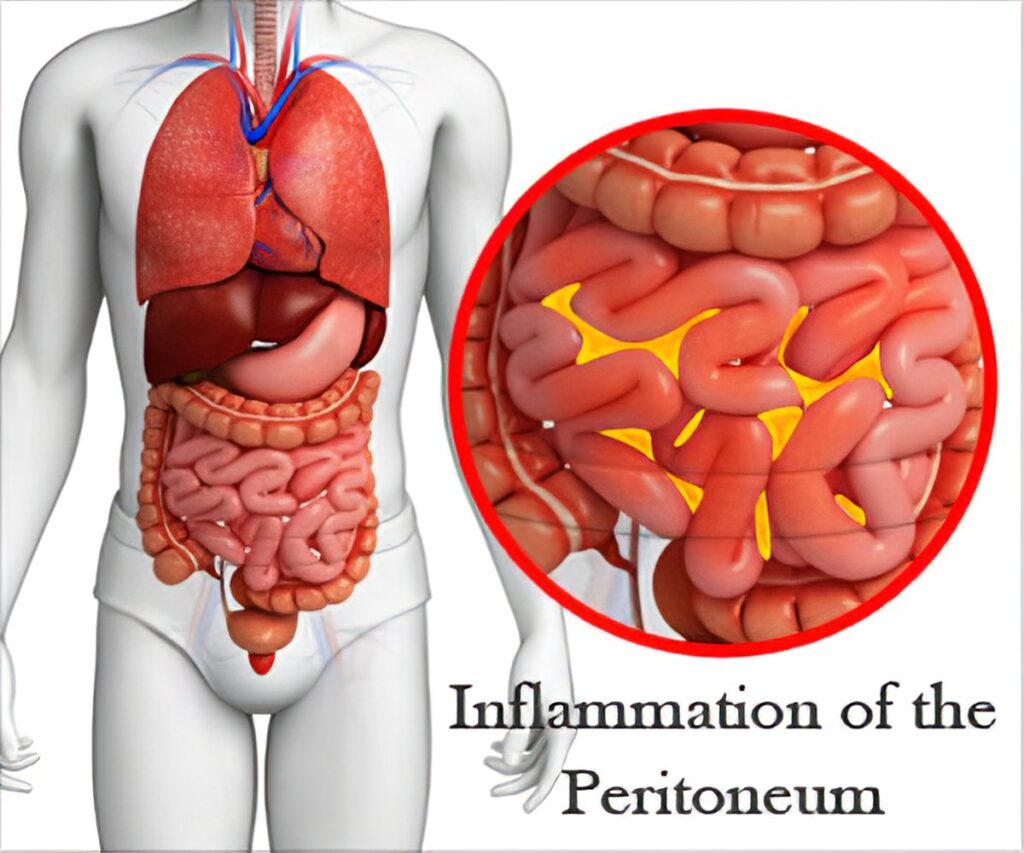
Peritonitis caused by Pseudomonas aeruginosa presents a significant medical challenge, particularly in patients undergoing peritoneal dialysis (PD). This type of infection is characterized by severe complications and requires prompt diagnosis and aggressive treatment. In this article, we will delve into the complexities of complicated Pseudomonas aeruginosa peritonitis, offering insights into its causes, clinical presentation, diagnostic strategies, and current treatment options.
What is Pseudomonas Aeruginosa Peritonitis?
Pseudomonas aeruginosa is a gram-negative bacterium commonly found in hospital environments, particularly in patients with compromised immune systems or underlying chronic conditions. This bacterium is notorious for its ability to form biofilms and develop resistance to multiple antibiotics. When P. aeruginosa infects the peritoneal cavity, it can lead to peritonitis, an inflammation of the peritoneum that can range from mild to severe.
Complicated vs. Uncomplicated Peritonitis
The term “complicated” in the context of peritonitis refers to infections that involve significant challenges in terms of treatment, recovery, or risk of sepsis. Complicated peritonitis is often associated with:
- Multi-drug resistant (MDR) organisms
- Abdominal abscesses or fluid collections
- Rapid progression to sepsis
- Delayed response to antibiotic therapy
In contrast, uncomplicated peritonitis typically resolves with prompt antibiotic treatment and is characterized by fewer complications.
Causes and Risk Factors
Source of Infection
Pseudomonas aeruginosa is commonly introduced into the peritoneum via contamination of the peritoneal dialysis catheter or as a result of abdominal surgery. Other potential sources include:
- Gastrointestinal perforations
- Appendicitis
- Diverticulitis
- Post-surgical infections
In patients on peritoneal dialysis, the risk of infection is heightened due to the continuous exposure of the peritoneum to external environments. The catheter site serves as a potential entry point for pathogens, including P. aeruginosa.
Risk Factors for Complicated Infection
Several factors increase the risk of developing complicated Pseudomonas aeruginosa peritonitis:
- Previous antibiotic use: This can lead to the development of resistant strains.
- Chronic kidney disease (CKD): Patients on dialysis have compromised immune function and are more prone to infections.
- Advanced age: Older patients often have a reduced immune response.
- Presence of comorbidities: Conditions such as diabetes mellitus, liver cirrhosis, and cancer can further predispose patients to infections.
- Use of immunosuppressive medications: These drugs can impair the body’s ability to fight infections, making dialysis patients more susceptible to severe infections like peritonitis.
Clinical Presentation of Complicated Pseudomonas Aeruginosa Peritonitis
Symptoms
The symptoms of complicated Pseudomonas aeruginosa peritonitis may present gradually or escalate rapidly. Common signs and symptoms include:
- Abdominal pain and tenderness
- Fever and chills
- Nausea and vomiting
- Loss of appetite
- Increased dialysate turbidity (in peritoneal dialysis patients)
In more severe cases, patients may develop signs of sepsis, including hypotension, tachycardia, and altered mental status.
Laboratory Findings
Laboratory investigations are crucial for diagnosing peritonitis. Key diagnostic tests include:
- Peritoneal fluid culture: Positive culture for Pseudomonas aeruginosa confirms the diagnosis.
- Blood cultures: These may also be positive, particularly in cases of sepsis.
- White blood cell count: Elevated levels can indicate infection.
- Lactate levels: Elevated lactate may suggest sepsis or tissue hypoxia, both of which are complications of complicated peritonitis.
Diagnostic Approach
Clinical Diagnosis
Clinicians often rely on a combination of patient history, clinical symptoms, and physical examination to suspect peritonitis. For patients on peritoneal dialysis, peritoneal fluid analysis remains the gold standard for confirming the infection.
Microbiological Diagnosis
Once Pseudomonas aeruginosa is suspected, peritoneal fluid should be sent for Gram stain, culture, and susceptibility testing. The bacterium’s ability to develop resistance to antibiotics makes susceptibility testing vital for determining effective treatment options.
Imaging Studies
In cases of complicated peritonitis, imaging studies such as abdominal ultrasound or CT scans may be used to assess the extent of the infection, identify abscesses, and evaluate the condition of the peritoneum.
Treatment of Complicated Pseudomonas Aeruginosa Peritonitis
Antibiotic Therapy
Given the prevalence of multi-drug resistance in Pseudomonas aeruginosa, effective antibiotic therapy is a cornerstone of treatment. Initial empiric therapy should cover broad-spectrum gram-negative bacteria while awaiting culture results. Commonly used antibiotics include:
- Ceftazidime or cefepime (third- or fourth-generation cephalosporins)
- Piperacillin-tazobactam (for broader coverage)
- Meropenem (for multi-drug resistant strains)
Once culture results are available, the regimen can be narrowed down based on the specific susceptibility pattern of the isolated organism.
Peritoneal Dialysis and Catheter Management
In patients on peritoneal dialysis, the catheter site should be thoroughly cleaned, and the catheter may need to be replaced if the infection does not resolve with antibiotic therapy alone. In severe cases, temporary cessation of dialysis may be required while intravenous antibiotics are administered.
Surgical Intervention
In cases where complicated peritonitis leads to the formation of abscesses or if there is bowel perforation, surgical intervention may be necessary. Drainage of abscesses or repair of the underlying anatomical issue may be required to resolve the infection.
Supportive Care
Supportive measures, such as intravenous fluids, vasopressors (for hypotension), and oxygen therapy (for patients with respiratory distress), are critical in managing sepsis associated with complicated peritonitis.
Prognosis
The prognosis for patients with complicated Pseudomonas aeruginosa peritonitis depends on several factors, including the timeliness of diagnosis, the patient’s immune status, and the presence of other comorbid conditions. Early diagnosis and appropriate antibiotic therapy are essential for improving outcomes. However, patients with resistant strains, delayed diagnosis, or extensive abdominal involvement face a higher risk of mortality.
Preventive Measures
Preventing Pseudomonas aeruginosa peritonitis, especially in dialysis patients, involves strict adherence to infection control measures, such as:
- Proper catheter care and hygiene
- Regular monitoring for signs of infection
- Prompt treatment of any abdominal issues, including gastrointestinal perforations or appendicitis
Prevention in Peritoneal Dialysis Patients
Peritoneal dialysis patients are particularly vulnerable to Pseudomonas aeruginosa infections. Education on the importance of hand hygiene, aseptic technique during dialysis exchanges, and catheter maintenance can significantly reduce the risk of peritonitis.