Proteus peritonitis, a severe form of abdominal infection, is associated with significant morbidity and mortality, especially in patients undergoing peritoneal dialysis. This bacterial infection is caused by Proteus species, commonly Proteus mirabilis, and can present in both simple and complicated forms. While the simple form is typically manageable with appropriate antibiotic therapy, complicated Proteus peritonitis requires more intensive management due to its potential to lead to significant complications such as sepsis, abscess formation, and even organ failure.
In this article, we provide a comprehensive examination of complicated Proteus peritonitis, including its pathophysiology, clinical presentation, diagnosis, treatment options, and preventive measures.
Pathophysiology of Proteus Peritonitis
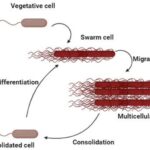
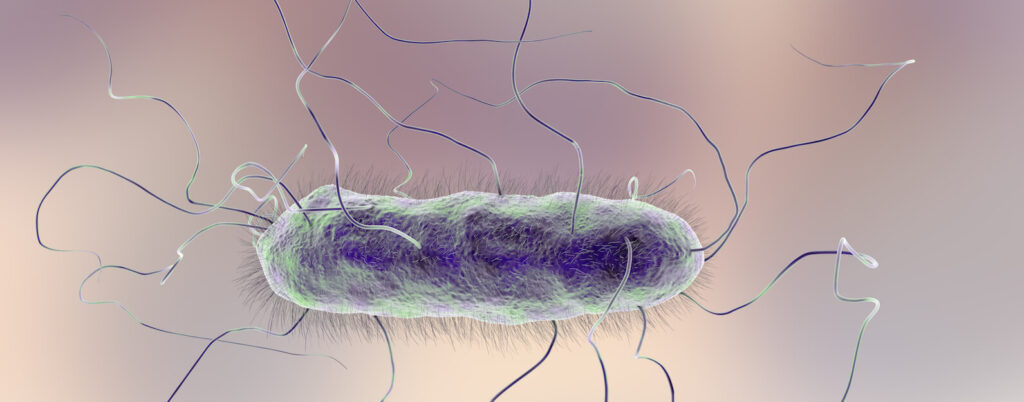
Proteus species are gram-negative bacteria commonly found in the gastrointestinal and genitourinary tracts. The pathogenicity of Proteus in peritonitis is often linked to its ability to produce urease, an enzyme that breaks down urea into ammonia and carbon dioxide, which can disrupt the normal pH balance of the peritoneal cavity and promote bacterial growth.
In peritoneal dialysis patients, the risk of infection increases due to the presence of a catheter, which can serve as a direct portal of entry for bacteria. In cases of complicated peritonitis, the infection may spread beyond the peritoneal cavity, leading to systemic involvement, including bacteremia and sepsis.
Clinical Manifestations of Complicated Proteus Peritonitis
The symptoms of complicated Proteus peritonitis can be severe and rapidly progressive. Key clinical signs include:
- Abdominal pain: Often sudden and intense, particularly around the peritoneal catheter site.
- Abdominal tenderness and distension: Increased sensitivity upon palpation and visible swelling.
- Fever and chills: Indicative of systemic involvement and potential sepsis.
- Nausea and vomiting: Common signs of intra-abdominal infection.
- Cloudy dialysate fluid: A hallmark of peritoneal dialysis-related peritonitis, typically presenting as a sign of infection.
Patients may also exhibit signs of systemic toxicity, including hypotension, tachycardia, and altered mental status, indicating a more severe infection.
Diagnosis of Complicated Proteus Peritonitis
The diagnosis of Proteus peritonitis is primarily clinical, supported by laboratory findings and microbiological cultures. Key diagnostic steps include:
1. Clinical Evaluation
A thorough physical examination and assessment of the patient’s symptoms and medical history are essential for identifying potential cases of peritonitis, especially in dialysis-dependent patients.
2. Microbiological Culture
Peritoneal fluid obtained via peritoneal dialysis catheter is cultured to identify the causative organism. The identification of Proteus mirabilis is confirmed through Gram stain and subsequent culture in appropriate media. Blood cultures may also be necessary in cases with suspected bacteremia or sepsis.
3. Imaging
While not always necessary, abdominal ultrasound or CT scans may be used to detect complications such as abscess formation, free air, or bowel perforation, which may indicate more complicated cases of peritonitis.
Treatment of Complicated Proteus Peritonitis
1. Antibiotic Therapy
Antibiotic therapy is the cornerstone of treatment for Proteus peritonitis. Empiric therapy should cover a broad spectrum of potential pathogens, with a focus on Gram-negative organisms, until culture results are available. Once Proteus is identified, treatment can be narrowed to target the specific pathogen. Commonly used antibiotics include:
- Third-generation cephalosporins: Such as ceftriaxone or cefotaxime.
- Aminoglycosides: Gentamicin or tobramycin may be used in combination with other antibiotics for synergy.
- Carbapenems: In more severe or resistant cases, meropenem or imipenem may be indicated.
It is important to adjust the antibiotic regimen based on sensitivity testing to avoid unnecessary use of broad-spectrum antibiotics.
2. Peritoneal Dialysis Modifications
For patients on peritoneal dialysis, discontinuation of the dialysis regimen is often necessary, and temporary hemodialysis may be initiated in cases of renal failure or complications from peritonitis. The peritoneal dialysis catheter should be assessed for signs of infection, and in some cases, removal may be required if the infection cannot be controlled.
3. Surgical Intervention
In severe cases, particularly when there is evidence of bowel perforation, abscess formation, or peritoneal contamination that cannot be controlled by antibiotics alone, surgical intervention may be required. This may involve drainage of abscesses, repair of perforated bowel, or other necessary procedures.
4. Supportive Care
Patients with complicated peritonitis often require intensive supportive care. This may include intravenous fluids to maintain blood pressure, vasopressors in cases of shock, and monitoring for signs of multi-organ failure.
Complications of Proteus Peritonitis
Complicated Proteus peritonitis can lead to several severe complications, including:
- Sepsis: A systemic inflammatory response to infection that can lead to organ failure and death if untreated.
- Abscess Formation: Localized collections of pus that may require surgical drainage.
- Bowel Perforation: A rare but life-threatening complication requiring emergency surgery.
- Chronic Peritoneal Inflammation: Prolonged infection can lead to scarring and fibrosis, potentially impairing the function of peritoneal dialysis.
Prevention Strategies
Preventing Proteus peritonitis, especially in patients undergoing peritoneal dialysis, is crucial. Key preventive measures include:
- Strict hygiene practices: Both patients and healthcare providers should follow rigorous aseptic techniques when handling peritoneal dialysis catheters.
- Antibiotic prophylaxis: Preemptive antibiotic therapy may be administered during catheter insertion or in cases of suspected infection.
- Regular monitoring: Frequent monitoring of peritoneal fluid for signs of infection can help detect peritonitis early, before it becomes complicated.
- Catheter care and maintenance: Regular cleaning and proper catheter care can reduce the risk of infection.
Prognosis of Complicated Proteus Peritonitis
The prognosis of complicated Proteus peritonitis depends on several factors, including the patient’s overall health, the timeliness of treatment, and the presence of underlying comorbidities. Early recognition and intervention significantly improve outcomes, but delayed treatment or inadequate management can result in severe complications, prolonged hospitalization, or even death.