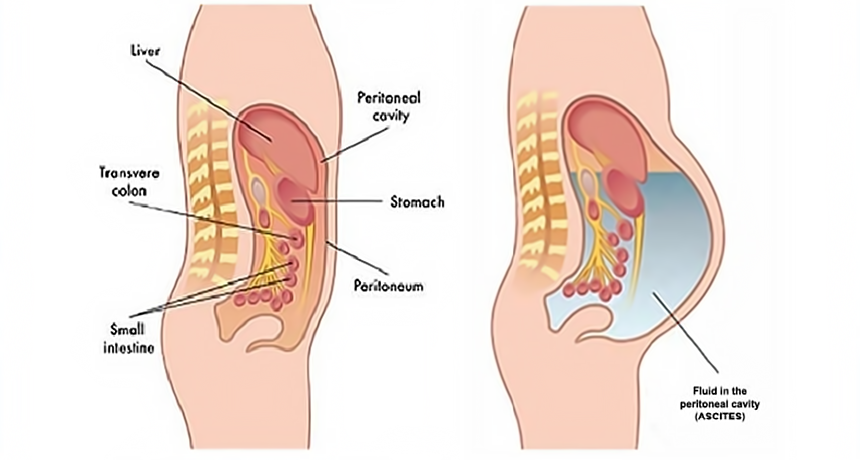
Peritonitis, an inflammation of the peritoneum, the membrane lining the abdominal cavity, is a serious medical condition. When complicated by Clostridium species, the infection can become particularly severe, posing a significant risk to the patient’s health. This article will delve into the complex nature of Clostridium-induced peritonitis, exploring its pathophysiology, clinical manifestations, diagnostic strategies, treatment options, and the prognosis for affected individuals.
What is Complicated Peritonitis?
Complicated peritonitis occurs when the infection causes extensive inflammation and affects surrounding structures, often leading to sepsis, multi-organ failure, or abscess formation. Clostridium, a genus of bacteria known for its ability to thrive in anaerobic environments, can be a major causative agent in such cases, further complicating the condition due to the fast-acting nature of these microorganisms.
Clostridium Species in Peritonitis
Clostridium species, particularly Clostridium perfringens, Clostridium difficile, and Clostridium septicum, are implicated in severe cases of peritonitis. These bacteria are anaerobic and produce potent toxins that can exacerbate the severity of the infection. Their involvement in peritonitis often results in more difficult-to-treat scenarios due to their aggressive nature and ability to cause rapid tissue destruction.
- Clostridium perfringens: Known for causing gas gangrene, C. perfringens can rapidly proliferate in the peritoneal cavity, leading to tissue necrosis and widespread infection.
- Clostridium difficile: While primarily known for causing antibiotic-associated colitis, C. difficile can also lead to peritonitis in patients with compromised gastrointestinal integrity.
- Clostridium septicum: Frequently associated with gastrointestinal malignancies, C. septicum can complicate peritonitis through the release of potent exotoxins, contributing to further tissue destruction and sepsis.
Causes and Risk Factors
Clostridium-induced peritonitis is often associated with specific risk factors and conditions that compromise the integrity of the gastrointestinal system. The most common causes include:
- Bowel Perforations: A perforated appendix, colon, or small intestine creates an entry point for bacteria like Clostridium to enter the peritoneal cavity.
- Trauma or Surgery: Abdominal trauma or surgical procedures that breach the peritoneum, such as bowel surgery, can introduce Clostridium species into the sterile abdominal cavity.
- Peritoneal Dialysis: Patients undergoing peritoneal dialysis are at increased risk of bacterial peritonitis, including infections caused by Clostridium.
- Pre-existing Gastrointestinal Disease: Conditions such as diverticulitis, colorectal cancer, and Crohn’s disease can predispose individuals to Clostridium peritonitis by providing pathways for bacteria to invade the peritoneum.
Symptoms of Clostridium-Induced Peritonitis
The symptoms of complicated peritonitis due to Clostridium infections are typically severe and escalate quickly. Key clinical manifestations include:
- Severe Abdominal Pain: Often localized or diffuse, pain is a hallmark symptom and may be accompanied by distension and tenderness.
- Fever and Chills: Systemic inflammatory response to the infection can lead to elevated body temperature, often with chills.
- Nausea and Vomiting: These symptoms are common due to the involvement of the gastrointestinal system.
- Signs of Sepsis: In advanced cases, patients may experience hypotension, tachycardia, and confusion, indicating the onset of sepsis.
- Foul-smelling Drainage: In cases of abscess formation, drainage from the abdominal cavity may have a characteristic, foul odor due to the anaerobic nature of Clostridium species.
Diagnosis of Complicated Peritonitis Due to Clostridium
Early and accurate diagnosis is critical in managing complicated peritonitis effectively. The following diagnostic tools and tests are commonly employed:
Clinical Examination and History
A thorough clinical examination, including the assessment of abdominal tenderness, distension, and signs of peritoneal irritation, is essential. Patient history, including prior surgeries, trauma, or conditions like diverticulitis, helps identify potential risk factors.
Imaging Studies
- Abdominal X-rays: Free air or gas in the peritoneal cavity, indicative of a perforation, can be detected on an X-ray.
- CT Scan: A contrast-enhanced CT scan is the gold standard for diagnosing intra-abdominal abscesses, bowel perforations, and the extent of the infection.
- Ultrasound: Useful in identifying fluid collections or abscesses in the peritoneum, though less detailed than CT scans.
Microbiological Cultures
- Peritoneal Fluid Cultures: Aspiration of peritoneal fluid through paracentesis allows for the identification of Clostridium species.
- Blood Cultures: In suspected septicemia, blood cultures are critical for identifying the pathogen and determining the most effective antibiotic regimen.
Treatment of Clostridium Peritonitis
Treatment of Clostridium-induced peritonitis requires a multifaceted approach involving surgery, antimicrobial therapy, and supportive care. Immediate intervention is vital due to the rapid progression of the infection.
Surgical Intervention
- Source Control: In many cases, surgical intervention is necessary to remove the source of infection, such as a perforated bowel, abscesses, or necrotic tissue. Surgery may involve resection of the affected bowel or drainage of abscesses.
- Debridement: Removal of necrotic tissue, particularly in cases of C. perfringens infections, is essential to prevent further spread of the bacteria.
Antibiotic Therapy
- Empiric Antibiotics: Broad-spectrum antibiotics, often including beta-lactam/beta-lactamase inhibitors or carbapenems, are initially administered to cover a wide range of possible pathogens, including Clostridium.
- Targeted Therapy: Once the specific Clostridium species is identified, antibiotic therapy is adjusted accordingly. For C. perfringens and C. septicum, penicillin G is commonly used, while C. difficile infections are treated with oral vancomycin or fidaxomicin.
Supportive Care
- Fluid Resuscitation: Intravenous fluids are essential to manage dehydration, electrolyte imbalances, and hypotension.
- Nutritional Support: Parenteral or enteral nutrition is provided, particularly if surgery has compromised the patient’s ability to absorb nutrients.
Prognosis and Complications
The prognosis for patients with complicated peritonitis due to Clostridium depends on several factors, including the timeliness of treatment, the patient’s overall health, and the extent of the infection. With prompt surgical intervention and appropriate antibiotic therapy, many patients can recover; however, the condition is often fatal in untreated cases due to the rapid progression to sepsis and organ failure.
Complications
- Sepsis: A systemic inflammatory response that can lead to multi-organ failure and death.
- Abscess Formation: Clostridium-induced peritonitis often leads to the formation of intra-abdominal abscesses, requiring drainage.
- Chronic Digestive Issues: Long-term complications may include bowel dysfunction or the need for permanent ostomies.