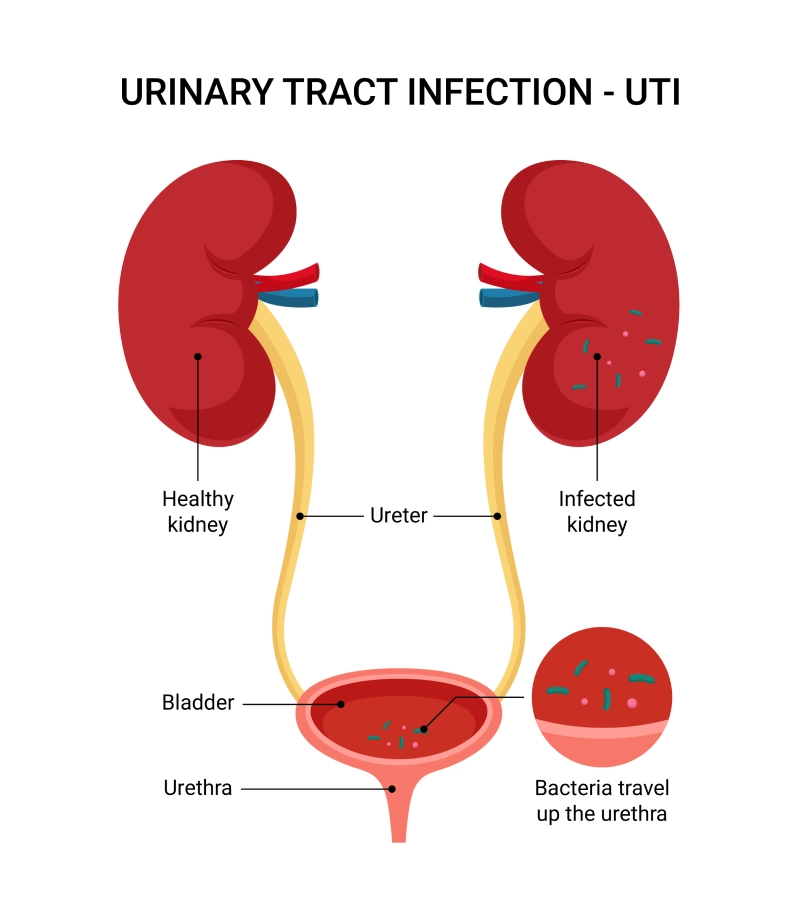
Complicated genitourinary tract infections (cUTIs) represent a significant concern in clinical practice due to their association with structural or functional abnormalities of the genitourinary system. These infections pose challenges in diagnosis and management, often leading to increased morbidity and healthcare costs. A thorough understanding of their etiology, risk factors, clinical presentation, diagnostic modalities, and treatment options is essential for effective patient care.
Etiology and Risk Factors
cUTIs are primarily caused by a diverse range of pathogens, with Escherichia coli being the most prevalent. However, other organisms such as Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas aeruginosa, and enterococci are also implicated. The presence of structural abnormalities, such as urinary obstruction, urolithiasis, or indwelling catheters, significantly increases the risk of infection. Functional impairments, including neurogenic bladder and vesicoureteral reflux, further predispose individuals to cUTIs. Additionally, immunocompromised states, such as diabetes mellitus and renal transplantation, contribute to the susceptibility and complexity of these infections.
Clinical Manifestations
The clinical presentation of cUTIs varies widely, ranging from asymptomatic bacteriuria to severe systemic manifestations like sepsis. Common symptoms include dysuria, frequency, urgency, hematuria, and suprapubic or flank pain. In cases involving upper urinary tract involvement, patients may exhibit fever, chills, and costovertebral angle tenderness. The presence of underlying abnormalities often complicates the clinical picture, necessitating a high index of suspicion for timely diagnosis.
Diagnostic Approaches
Accurate diagnosis of cUTIs involves a combination of clinical assessment, laboratory investigations, and imaging studies. Urinalysis typically reveals pyuria and bacteriuria, while urine culture remains the gold standard for identifying causative organisms and determining antimicrobial susceptibility. Blood cultures may be warranted in patients with systemic symptoms to assess for bacteremia. Imaging modalities, such as ultrasound or computed tomography (CT), are essential for detecting structural abnormalities, obstructions, or abscess formations that may necessitate surgical intervention.
Treatment Strategies
The management of cUTIs requires a multifaceted approach tailored to the individual patient. Empirical antibiotic therapy should be initiated promptly, guided by local resistance patterns and patient-specific factors. Definitive therapy is adjusted based on culture results and susceptibility profiles. The duration of antibiotic treatment is typically longer than that for uncomplicated UTIs, often extending to 10-14 days. Addressing underlying structural or functional abnormalities is crucial to prevent recurrence. This may involve surgical correction of obstructions, removal or replacement of indwelling devices, or management of metabolic disorders. Close monitoring and follow-up are essential to ensure resolution of the infection and to manage any potential complications.
Complicated genitourinary tract infections present significant diagnostic and therapeutic challenges due to their association with anatomical and functional abnormalities. A comprehensive understanding of their etiology, risk factors, clinical manifestations, and management strategies is essential for effective treatment and prevention of recurrence. Early recognition and prompt intervention, coupled with addressing underlying abnormalities, are pivotal in improving patient outcomes.