Enterobacter peritonitis represents a significant clinical challenge, particularly in patients undergoing peritoneal dialysis (PD). The emergence of multidrug-resistant (MDR) Enterobacter strains has further complicated management strategies, necessitating a comprehensive understanding of its pathogenesis, clinical manifestations, diagnostic approaches, and treatment options.
Pathogenesis of Enterobacter Peritonitis
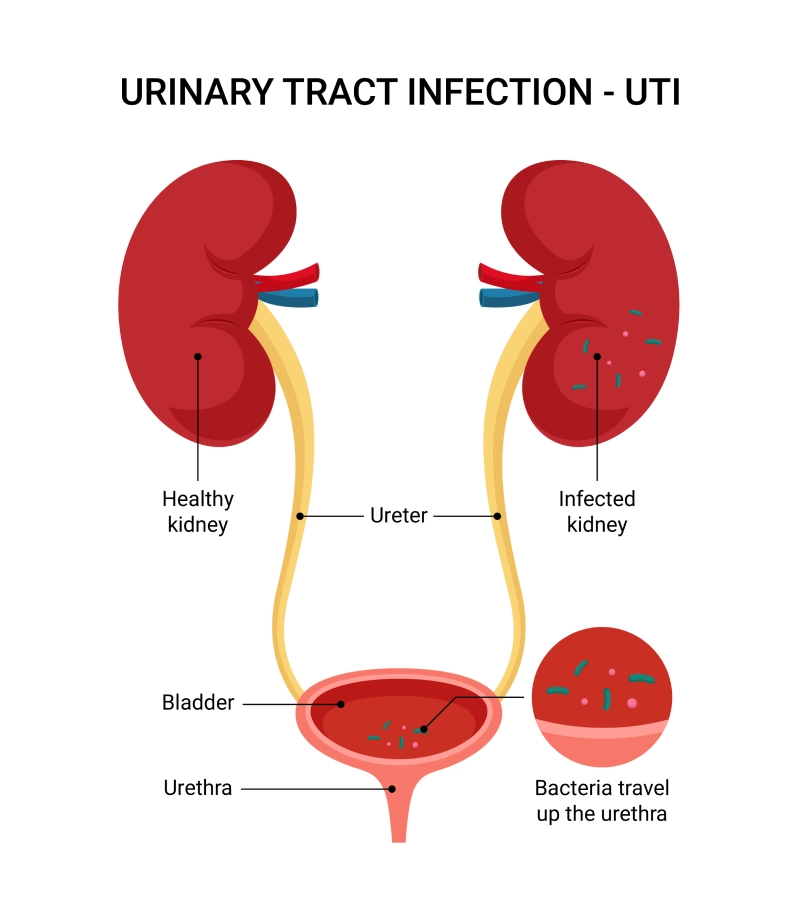
Enterobacter species are gram-negative, facultatively anaerobic bacilli commonly found in the gastrointestinal tract. Peritonitis caused by Enterobacter can occur through several mechanisms:
- Translocation: Bacterial migration from the gut lumen to the peritoneal cavity, often facilitated by increased intestinal permeability.
- Contamination: Introduction of bacteria during PD exchanges due to breaches in sterile technique.
- Hematogenous Spread: Dissemination from distant infection sites via the bloodstream.
The propensity of Enterobacter species to acquire resistance mechanisms, such as extended-spectrum beta-lactamases (ESBLs) and carbapenemases, complicates treatment and contributes to higher morbidity and mortality rates.
Clinical Manifestations
Patients with Enterobacter peritonitis typically present with:
- Abdominal Pain: Diffuse tenderness and discomfort.
- Cloudy Dialysate Effluent: Indicative of infection in PD patients.
- Fever: Elevated body temperature, though it may be absent in immunocompromised individuals.
- Gastrointestinal Symptoms: Nausea, vomiting, or diarrhea.
In severe cases, patients may develop septic shock, characterized by hypotension and organ dysfunction.
Diagnostic Approaches
Accurate and prompt diagnosis is crucial for effective management. Key diagnostic steps include:
- Peritoneal Fluid Analysis: Elevated white blood cell count (>100 cells/µL) with a predominance of polymorphonuclear cells suggests peritonitis.
- Microbiological Cultures: Isolation and identification of Enterobacter species from peritoneal fluid cultures confirm the diagnosis.
- Antibiotic Susceptibility Testing: Determines the resistance profile to guide targeted therapy.
Advanced molecular techniques, such as polymerase chain reaction (PCR), can detect specific resistance genes, aiding in the identification of MDR strains.
Treatment Strategies
Management of Enterobacter peritonitis involves a combination of antimicrobial therapy and supportive care:
- Empirical Antibiotic Therapy: Initiate broad-spectrum antibiotics covering gram-negative organisms, including potential ESBL-producing strains.
- Supportive Care: Includes fluid resuscitation, electrolyte management, and hemodynamic support as needed.
- Catheter Management: In PD patients, assess the need for catheter removal, especially in refractory cases or when the catheter is the suspected source of infection.
Early consultation with infectious disease specialists is recommended to optimize treatment outcomes.
Prevention and Prognosis
Preventive measures are essential to reduce the incidence of Enterobacter peritonitis:
- Aseptic Technique: Strict adherence during PD exchanges to prevent contamination.
- Patient Education: Training on proper exchange procedures and early recognition of infection signs.
- Regular Monitoring: Routine follow-up and monitoring for potential complications.
The prognosis of Enterobacter peritonitis depends on factors such as the patient’s overall health, timeliness of diagnosis, and appropriateness of therapy. MDR strains are associated with higher treatment failure rates and mortality, underscoring the importance of early detection and appropriate antimicrobial therapy.
Complicated Enterobacter peritonitis presents significant challenges due to its potential for severe outcomes and the increasing prevalence of MDR strains. A thorough understanding of its pathogenesis, clinical presentation, and management strategies is vital for healthcare providers to improve patient outcomes.