Complicated bacterial peritonitis is a severe and potentially life-threatening condition that requires immediate medical attention. It occurs when the peritoneum, the thin membrane lining the abdominal cavity and covering the organs within it, becomes infected. This condition is commonly seen in patients undergoing peritoneal dialysis but can affect individuals with underlying abdominal pathologies. In this article, we explore the intricate details of complicated bacterial peritonitis, its pathophysiology, diagnosis, and treatment strategies.
What Is Complicated Bacterial Peritonitis?
Complicated bacterial peritonitis is characterized by a bacterial infection in the peritoneum that leads to widespread inflammation. Unlike simple peritonitis, complicated cases often involve the presence of abscesses, septic shock, or other severe complications. These infections can originate from various sources, including ruptured organs, perforations in the gastrointestinal tract, or infections associated with peritoneal dialysis.
Pathophysiology of Bacterial Peritonitis
The infection typically starts when bacteria enter the peritoneal cavity, either through the bloodstream or from an external source. Once inside, the bacteria multiply, causing inflammation and triggering the body’s immune response. In complicated cases, the infection spreads to the surrounding tissues, leading to tissue necrosis and the formation of abscesses. If left untreated, this can lead to sepsis and organ failure, making prompt diagnosis and treatment crucial.
Common Causes of Complicated Bacterial Peritonitis
There are several potential causes of complicated bacterial peritonitis. The most common include:
- Peritoneal Dialysis: Bacterial peritonitis is a frequent complication in patients undergoing peritoneal dialysis. The peritoneal catheter provides a direct route for bacteria to enter the abdominal cavity, increasing the risk of infection.
- Gastrointestinal Perforations: A perforation in the gastrointestinal tract (e.g., from a ruptured appendix, diverticulum, or peptic ulcer) can lead to the leakage of intestinal contents into the peritoneum, resulting in bacterial infection.
- Abdominal Surgery: Post-operative infections are a significant risk factor for peritonitis, particularly when the abdominal cavity is exposed during surgery.
- Trauma or Injury: Physical injury to the abdominal area can introduce bacteria into the peritoneum, leading to infection.
- Spread from Other Infections: In some cases, infections from other areas of the body, such as the bloodstream or urinary tract, may spread to the peritoneum.
Symptoms of Complicated Bacterial Peritonitis
The symptoms of complicated bacterial peritonitis can vary, but they generally include:
- Severe Abdominal Pain: Often diffuse, the pain may become more localized as the infection progresses.
- Abdominal Tenderness: The abdomen may become rigid and tender to touch, especially in the affected area.
- Fever and Chills: These are common signs of systemic infection as the body attempts to fight the bacteria.
- Nausea and Vomiting: Due to the inflammation and disruption in the gastrointestinal system, patients may experience nausea and vomiting.
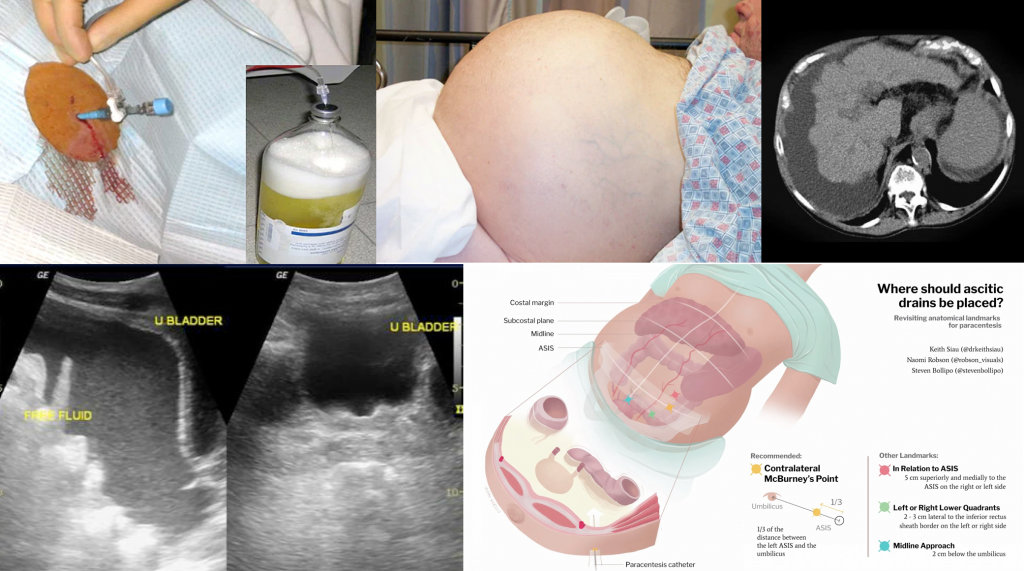
- Distended Abdomen: An accumulation of fluid in the abdomen (ascites) can occur, leading to bloating and discomfort.
- Signs of Sepsis: If the infection spreads to the bloodstream, patients may exhibit signs of sepsis, including low blood pressure, rapid heart rate, confusion, and organ dysfunction.
Diagnosing Complicated Bacterial Peritonitis
Accurate diagnosis of complicated bacterial peritonitis requires a combination of clinical evaluation, laboratory tests, and imaging studies. Key diagnostic steps include:
- Physical Examination: The physician will assess for signs of abdominal tenderness, rigidity, and distension.
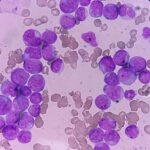
- Blood Tests: Elevated white blood cell count (leukocytosis), increased C-reactive protein (CRP), and other inflammatory markers may indicate an ongoing infection.
- Peritoneal Fluid Analysis: If peritoneal dialysis is being used, a sample of the peritoneal fluid is obtained for microbiological culture. In patients with spontaneous bacterial peritonitis, this can help identify the causative organism.
- Imaging: Abdominal ultrasound, CT scans, or X-rays can help detect fluid accumulation, abscesses, or perforations within the abdominal cavity.
Treatment of Complicated Bacterial Peritonitis
The management of complicated bacterial peritonitis is multifaceted and requires rapid intervention to prevent life-threatening complications. The main components of treatment include:
1. Antibiotic Therapy
Empirical antibiotic therapy is initiated immediately to target the most likely pathogens while awaiting culture results. Broad-spectrum antibiotics are typically used initially, followed by narrower antibiotics once the specific bacterial strain is identified. Commonly used antibiotics include:
- Ceftriaxone
- Piperacillin-tazobactam
- Vancomycin (in case of methicillin-resistant Staphylococcus aureus, MRSA)
- Metronidazole (for anaerobic infections)
2. Surgical Intervention
In cases where there is a perforated organ or abscess formation, surgery may be necessary. This could involve:
- Draining Abscesses: If abscesses have formed within the peritoneum, they must be drained to allow proper healing and reduce the spread of infection.
- Repairing Perforations: For gastrointestinal perforations, surgical repair is often required to close the perforated site and prevent further leakage of contaminants into the peritoneum.
3. Supportive Care
Supportive measures are critical, particularly for patients with sepsis or septic shock. These may include:
- Intravenous Fluids: To maintain blood pressure and support organ function.
- Vasopressors: In severe cases of septic shock, medications may be needed to increase blood pressure.
- Nutritional Support: Ensuring the patient receives adequate nutrition is crucial, especially if the gastrointestinal system is compromised.
4. Peritoneal Dialysis Management
For patients with peritoneal dialysis-associated bacterial peritonitis, the catheter may need to be removed, and antibiotic therapy should be adjusted. In severe cases, the patient may need to transition to hemodialysis.
Prevention of Complicated Bacterial Peritonitis
Prevention strategies are essential to reduce the incidence of complicated bacterial peritonitis, particularly in high-risk populations such as those undergoing peritoneal dialysis. These include:
- Proper Catheter Care: Ensuring strict hygiene and aseptic technique during catheter insertion and maintenance.
- Timely Treatment of Infections: Early intervention for gastrointestinal perforations, abdominal trauma, or infections can help prevent the spread of bacteria to the peritoneum.
- Vaccination: For patients with underlying conditions or those undergoing peritoneal dialysis, vaccinations against common pathogens may help reduce the risk of infection.