Colorectal perioperative infections present a significant challenge in surgical care, often leading to increased patient morbidity, prolonged hospital stays, and escalated healthcare costs. Understanding the key factors contributing to these infections, as well as the effective strategies for prevention and management, is essential for healthcare professionals involved in colorectal surgery. This guide explores the causes, prevention methods, and best practices for managing colorectal perioperative infections, providing crucial insights to optimize patient outcomes and reduce infection rates.
What is Colorectal Perioperative Infection?
A colorectal perioperative infection is a postoperative infection that occurs in patients undergoing colorectal surgery. These infections can affect the surgical wound, internal organs, or other parts of the body, leading to complications such as sepsis, delayed healing, or even death in severe cases. The types of infections associated with colorectal surgeries include surgical site infections (SSIs), intra-abdominal infections, and infections related to anastomotic leaks.
Causes and Risk Factors of Colorectal Perioperative Infection
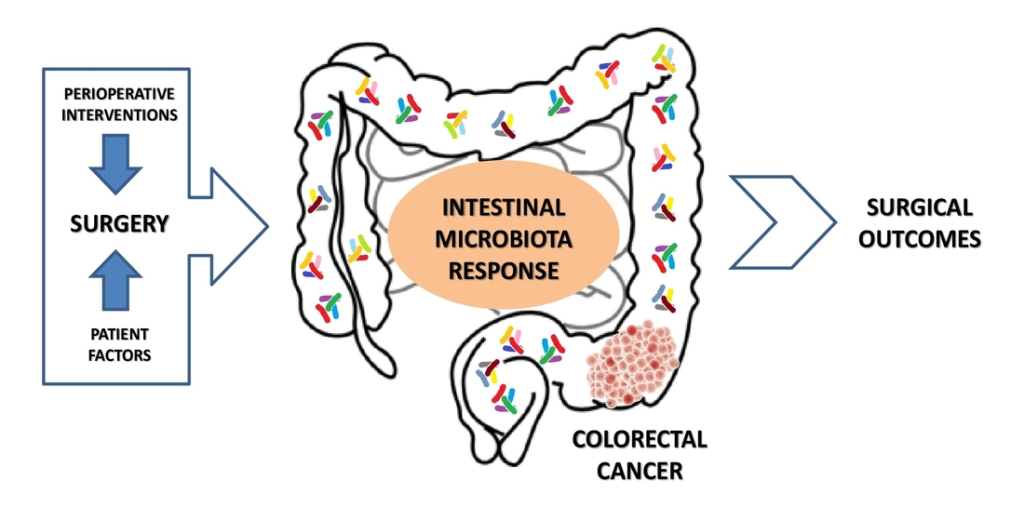
Several factors contribute to the development of colorectal perioperative infections. These include the patient’s underlying health conditions, the surgical procedure itself, and environmental factors such as surgical techniques and infection control protocols.
1. Bacterial Contamination During Surgery
The colon is home to a variety of bacteria, including Escherichia coli, Bacteroides fragilis, and Clostridium species. During colorectal surgery, these bacteria can enter the bloodstream, abdominal cavity, or surgical site, leading to infection. Proper surgical techniques, including aseptic procedures, are critical to minimizing the risk of contamination.
2. Immunocompromised Patients
Patients with compromised immune systems, due to conditions like diabetes, cancer, or immunosuppressive therapy, are at an increased risk for infections. These individuals have a reduced ability to fight off infections, making them more susceptible to perioperative infections.
3. Obesity and Malnutrition
Obesity and malnutrition both increase the risk of wound infection and poor wound healing. Obese patients often have increased tissue oxygen consumption and reduced blood flow to surgical sites, while malnourished patients have weakened immune responses that hinder infection resistance.
4. Longer Surgical Duration and Invasive Procedures
Prolonged surgeries and those involving complex procedures, such as bowel resections or anastomoses, provide more opportunities for bacterial contamination. These extended operations also increase the likelihood of tissue damage, which can complicate recovery and elevate infection risks.
5. Presence of Comorbidities
Conditions such as diabetes mellitus, heart disease, and chronic kidney disease can increase the likelihood of infection following colorectal surgery. These comorbidities can impair the body’s ability to heal and fight infections.
Effective Prevention Strategies for Colorectal Perioperative Infection
Preventing colorectal perioperative infections requires a multifaceted approach, including preoperative optimization, intraoperative measures, and postoperative care. By implementing evidence-based strategies, surgical teams can reduce infection rates and improve patient outcomes.
1. Antibiotic Prophylaxis
Administering prophylactic antibiotics before colorectal surgery is essential for reducing the risk of infection. Typically, broad-spectrum antibiotics such as cefazolin or ceftriaxone are used, with specific adjustments made based on patient allergies or infection risk factors. The timing of antibiotic administration is critical: antibiotics should be administered within one hour before the incision to ensure peak levels at the time of surgery.
2. Optimizing Nutritional Status
Ensuring that patients are well-nourished before surgery is a vital step in preventing infections. Protein supplementation and the management of comorbidities like diabetes can significantly improve immune function and wound healing. Malnourished patients should receive nutritional support before surgery to improve their ability to combat infection.
3. Surgical Site Preparation and Aseptic Techniques
Surgeons must follow strict aseptic techniques during colorectal surgeries to minimize bacterial contamination. This includes proper hand hygiene, sterilization of surgical instruments, and the use of sterile drapes. Additionally, hair removal from the surgical site should be avoided or done using clippers, not razors, to reduce the risk of microabrasions.
4. Minimizing Surgical Trauma
Minimizing tissue handling and using techniques that preserve blood flow to tissues during surgery can reduce the risk of infection. Surgeons should aim to reduce surgical duration where possible and utilize minimally invasive techniques such as laparoscopic surgery to minimize trauma and reduce the chances of infection.
5. Optimizing Blood Glucose Levels
Hyperglycemia during the perioperative period has been linked to an increased risk of infection. Maintaining optimal blood glucose control, especially in diabetic patients, helps to reduce the likelihood of infections and promotes better healing outcomes.
Management of Colorectal Perioperative Infection
Even with the best prevention strategies, some patients may still develop colorectal perioperative infections. Early detection and prompt treatment are essential to managing these infections effectively.
1. Early Diagnosis of Surgical Site Infections
Postoperative monitoring for signs of infection, including fever, redness, swelling, and drainage from the surgical site, is critical. Any suspected surgical site infection should be promptly evaluated using clinical examination, laboratory tests (such as a white blood cell count), and imaging studies if necessary.
2. Antibiotic Therapy
Once an infection is suspected, broad-spectrum antibiotics should be initiated. These antibiotics should be tailored based on the identified pathogens and their susceptibility profile. Cultures obtained from wound sites or intra-abdominal fluids help guide antibiotic therapy, ensuring targeted treatment.
3. Drainage and Debridement
In cases of abscess formation or anastomotic leaks, drainage or surgical debridement may be necessary to remove infected tissue and promote healing. The decision to proceed with drainage or debridement depends on the severity of the infection and the patient’s overall condition.
4. Management of Anastomotic Leaks
Anastomotic leaks are a serious complication that can lead to peritonitis and sepsis. These leaks must be identified early and managed with surgical revision, percutaneous drainage, or the use of stents to control the infection and allow the anastomosis to heal.
5. Supportive Care
Supportive care, including intravenous fluids, electrolyte balance, and pain management, is crucial for patients with colorectal perioperative infections. Patients should be closely monitored in an intensive care unit (ICU) setting if their condition worsens or if they develop systemic infections such as sepsis.
Postoperative Care and Wound Healing
Postoperative care plays a vital role in preventing and managing colorectal perioperative infections. Wound care should focus on maintaining a clean and dry surgical site, monitoring for any signs of infection, and ensuring early mobilization to prevent complications such as deep vein thrombosis (DVT).
1. Wound Care Protocols
Strict adherence to wound care protocols is necessary to prevent contamination. Dressing changes should be performed using aseptic techniques, and any signs of infection, such as increased drainage or erythema, should prompt immediate evaluation and intervention.
2. Patient Education
Educating patients about the importance of proper hygiene and wound care at home is essential for preventing postoperative infections. Patients should be instructed on how to recognize early signs of infection, when to seek medical attention, and how to care for their incisions to promote healing.

