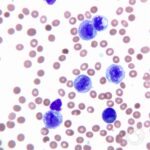
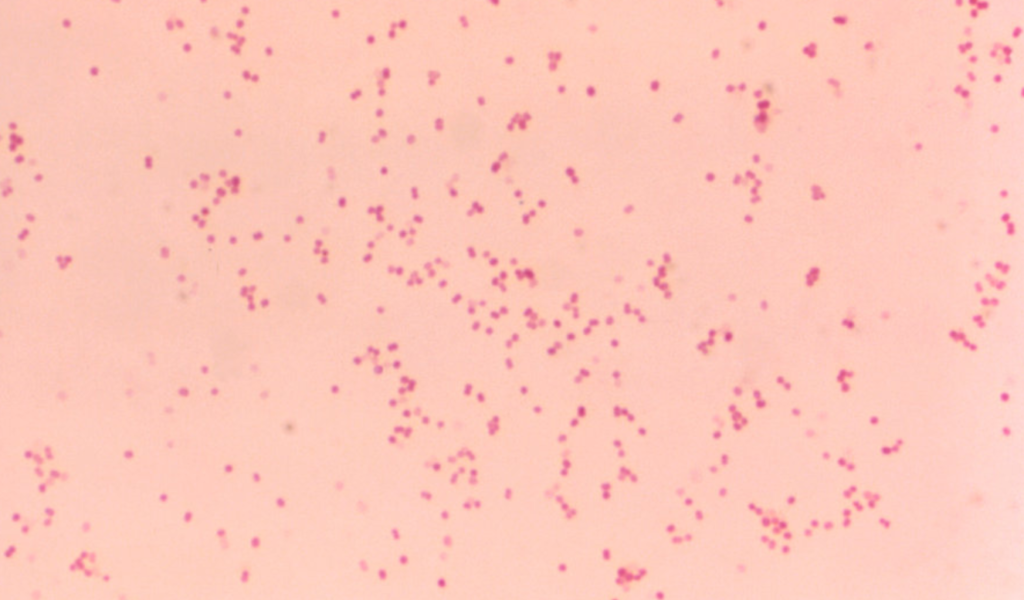
Acute Moraxella catarrhalis bacterial sinusitis is a common yet often overlooked cause of sinus infections, particularly in children and individuals with compromised immune systems. As a Gram-negative, aerobic diplococcus, M. catarrhalis colonizes the respiratory tract and can lead to persistent inflammation, nasal congestion, and secondary infections. Understanding the pathophysiology, risk factors, symptoms, and treatment options is crucial for effective management and prevention.
Pathophysiology of M. catarrhalis Sinus Infections
M. catarrhalis thrives in the upper respiratory tract, particularly in the nasopharynx, where it can persist asymptomatically. However, when the host’s immune defenses are weakened, the bacterium proliferates, leading to sinus inflammation, mucus overproduction, and secondary bacterial infections.
Risk Factors for Acute M. catarrhalis Sinusitis
Several conditions predispose individuals to developing sinus infections caused by M. catarrhalis:
- Weakened Immune System: Patients with chronic illnesses or immunodeficiencies.
- Frequent Upper Respiratory Infections: Common colds or flu can facilitate bacterial overgrowth.
- Allergic Rhinitis: Chronic nasal inflammation promotes bacterial retention.
- Exposure to Air Pollution: Irritants damage the mucosal barrier.
- Smoking and Second-Hand Smoke: Compromises respiratory defenses.
- Prolonged Antibiotic Use: Can alter microbiome balance, promoting bacterial resistance.
Clinical Symptoms
Acute bacterial sinusitis due to M. catarrhalis presents with:
- Nasal Congestion: Persistent blockage affecting breathing.
- Purulent Nasal Discharge: Thick, yellow-green mucus.
- Facial Pain and Pressure: Especially around the forehead, cheeks, and eyes.
- Headache: Worsens with bending forward.
- Postnasal Drip: Causes throat irritation and cough.
- Fever and Malaise: Indicative of bacterial infection.
Diagnosis
Accurate diagnosis requires:
- Clinical Examination: Assessing sinus tenderness, nasal inflammation, and symptoms.
- Nasal Swab Culture: Identifies M. catarrhalis as the causative agent.
- Computed Tomography (CT) Scan: Evaluates sinus blockage and complications.
- Blood Tests: Helps differentiate bacterial from viral infections.
Treatment Strategies
1. Antibiotic Therapy
- First-line antibiotics: Amoxicillin-clavulanate, cephalosporins, or macrolides (azithromycin, clarithromycin).
- Beta-lactamase inhibitors: Address antibiotic resistance.
- Alternative treatments: Fluoroquinolones in severe cases.
2. Symptomatic Relief
- Nasal Decongestants: Reduce swelling (e.g., oxymetazoline for short-term use).
- Saline Nasal Irrigation: Clears mucus buildup.
- Pain Relievers: Ibuprofen or acetaminophen for symptom relief.
3. Surgical Intervention
For recurrent or chronic cases unresponsive to medication:
- Functional Endoscopic Sinus Surgery (FESS): Removes obstructions and improves drainage.
- Balloon Sinuplasty: Less invasive procedure for sinus dilation.
Prevention Strategies
- Vaccination: Pneumococcal and influenza vaccines reduce infection risk.
- Good Nasal Hygiene: Regular saline irrigation prevents bacterial buildup.
- Avoid Smoking and Pollutants: Protects sinus mucosa.
- Manage Allergies: Reduces inflammation and bacterial retention.
- Early Treatment of Upper Respiratory Infections: Prevents progression to bacterial sinusitis.
Prognosis and Complications
While most cases resolve with appropriate treatment, untreated bacterial sinusitis can lead to:
- Orbital Cellulitis: Infection spreading to the eye socket.
- Meningitis: Rare but severe complication if bacteria reach the central nervous system.
- Chronic Sinusitis: Persistent inflammation requiring prolonged management.
- Hearing Loss (in Children): Due to middle ear infections associated with M. catarrhalis.
Acute Moraxella catarrhalis bacterial sinusitis is a significant cause of sinus infections, particularly in vulnerable populations. Prompt diagnosis, targeted antibiotic therapy, and preventive measures can effectively manage and reduce recurrence. Public awareness and improved clinical strategies remain vital in combating this condition.