Acute maxillary sinusitis, commonly referred to as a sinus infection, is an inflammation of the maxillary sinuses, often resulting from bacterial pathogens. Among these, Streptococcus pneumoniae is a predominant causative agent. This article delves into the pathophysiology, clinical manifestations, diagnostic approaches, and management strategies for acute maxillary Streptococcus pneumoniae sinusitis.
Pathophysiology of Acute Maxillary Sinusitis
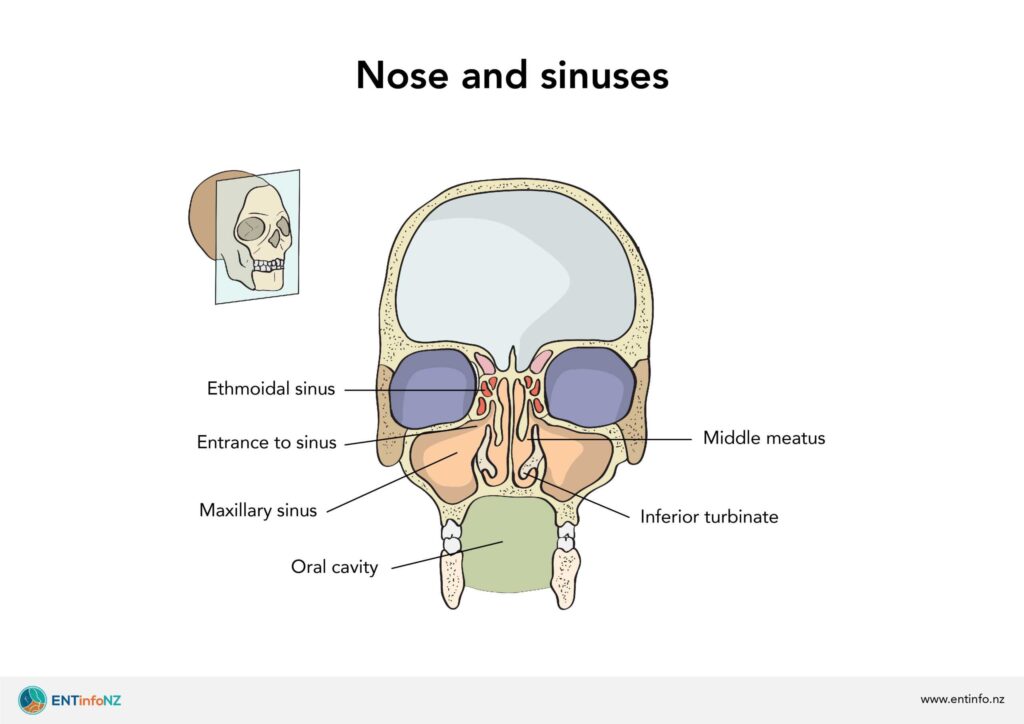
The maxillary sinuses, located beneath the eyes, are susceptible to infection when the sinus ostium becomes obstructed, leading to the retention of secretions and a favorable environment for bacterial growth. Streptococcus pneumoniae, a gram-positive, catalase-negative, facultatively anaerobic coccus, is a leading pathogen in acute bacterial rhinosinusitis.
Clinical Manifestations
Patients with acute maxillary Streptococcus pneumoniae sinusitis typically present with:
- Nasal Congestion: Obstruction of nasal passages due to inflammation.
- Purulent Nasal Discharge: Thick, yellow or green mucus indicating bacterial infection.
- Facial Pain or Pressure: Particularly over the maxillary sinuses.
- Headache: Often localized to the frontal region.
- Fever: May be present, especially in more severe cases.
- Cough: Typically worse at night.
In children, additional symptoms such as fetid breath and irritability may be observed.
Diagnostic Approaches
Diagnosis of acute maxillary Streptococcus pneumoniae sinusitis involves:
- Clinical Evaluation: Assessment of symptoms and physical examination findings.
- Imaging Studies: Computed tomography (CT) or magnetic resonance imaging (MRI) can reveal sinus opacification.
- Microbiological Cultures: Obtaining sinus aspirates to identify the causative organism.
Studies have shown that patients infected with Streptococcus pneumoniae exhibit more severe disease and total opacity on imaging compared to those infected with Haemophilus influenzae.
Management Strategies
Treatment of acute maxillary Streptococcus pneumoniae sinusitis includes:
- Antibiotic Therapy: First-line agents include amoxicillin or amoxicillin-clavulanate. In cases of penicillin-resistant S. pneumoniae, alternative antibiotics such as ceftriaxone or levofloxacin may be considered.
- Symptomatic Relief: Use of nasal decongestants, saline nasal irrigation, and analgesics to alleviate symptoms.
- Surgical Intervention: Indicated in cases unresponsive to medical therapy or in the presence of complications.
Prognosis
With appropriate treatment, the prognosis for acute maxillary Streptococcus pneumoniae sinusitis is generally favorable. However, delays in treatment or inadequate therapy can lead to complications such as orbital cellulitis, intracranial abscess, or chronic sinusitis.
Prevention
Preventive measures include:
- Vaccination: The pneumococcal vaccine can reduce the incidence of Streptococcus pneumoniae infections.
- Good Hygiene Practices: Regular handwashing and avoiding close contact with individuals exhibiting respiratory symptoms.
- Management of Allergies: Controlling allergic rhinitis to prevent sinus obstruction.
Acute maxillary Streptococcus pneumoniae sinusitis is a common yet potentially serious condition. Early recognition and appropriate management are crucial to prevent complications and ensure favorable outcomes. Healthcare providers should maintain a high index of suspicion and employ a comprehensive approach to diagnosis and treatment.