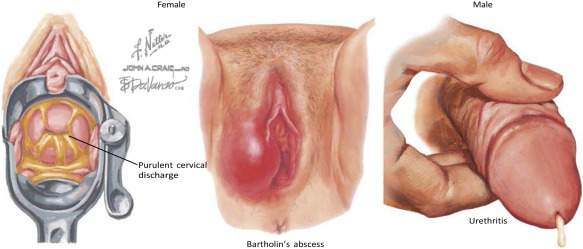
Acute lower genitourinary gonorrhea is a sexually transmitted infection (STI) caused by Neisseria gonorrhoeae, a gram-negative diplococcus. This condition primarily affects the urethra in males and the endocervix or urethra in females. Transmission occurs through unprotected sexual contact, with symptoms manifesting 2–7 days post-exposure. Left untreated, it may lead to severe complications, including pelvic inflammatory disease (PID), infertility, and disseminated gonococcal infection.
Clinical Presentation and Symptomatology
Key Symptoms in Males
- Dysuria (painful urination)
- Purulent urethral discharge
- Urethral itching or irritation
- Rare complications: epididymitis, prostatitis
Key Symptoms in Females
- Increased vaginal discharge
- Dysuria
- Intermenstrual bleeding
- Asymptomatic cases (up to 50%), increasing transmission risk
Pathophysiology of Gonococcal Infection
Neisseria gonorrhoeae adheres to mucosal surfaces via pili and opacity-associated proteins, invading epithelial cells and triggering localized inflammation. The pathogen’s ability to evade immune responses through antigenic variation complicates long-term immunity.
Diagnostic Approaches for Gonorrhea
Nucleic Acid Amplification Tests (NAATs)
NAATs are the gold standard for detecting Neisseria gonorrhoeae due to their high sensitivity (95–98%) and specificity. Samples are collected from urine, urethral, or endocervical sites.
Culture and Antimicrobial Susceptibility Testing
Culture remains critical for identifying antibiotic-resistant strains. Thayer-Martin agar is used for isolation, followed by disk diffusion or E-testing for resistance profiling.
Evidence-Based Treatment Protocols
First-Line Therapy
The CDC recommends dual therapy to combat resistance:
- Ceftriaxone (500 mg intramuscularly, single dose)
- Azithromycin (1 g orally, single dose)
Managing Resistance
Increasing resistance to cephalosporins necessitates vigilance. Alternative regimens, such as gentamicin + azithromycin, are reserved for allergic patients under strict monitoring.
Antibiotic Resistance: A Growing Threat
Global surveillance programs report rising resistance rates:
- 8% of isolates show reduced ceftriaxone susceptibility (2023 data)
- 65% resistance to ciprofloxacin in the US
Strategies to mitigate resistance include:
- Adherence to dual therapy guidelines
- Partner treatment and contact tracing
- Avoiding empiric monotherapy
Preventive Measures and Public Health Strategies
Individual Prevention
- Consistent condom use during sexual activity
- Regular STI screening for high-risk populations
- Expedited partner therapy (EPT) to reduce reinfection
Community-Level Interventions
- Public education campaigns targeting asymptomatic spread
- Enhanced surveillance in regions with high resistance rates
Complications of Untreated Gonorrhea
- Pelvic Inflammatory Disease (PID): 10–20% risk in untreated females
- Infertility: Tubal scarring in 8–10% of PID cases
- Disseminated Gonococcal Infection (DGI): Rare (<1%) but life-threatening
Combating acute lower genitourinary gonorrhea requires a multidisciplinary approach integrating rapid diagnostics, adherence to dual therapy, and robust public health initiatives. Ongoing research into vaccines and novel antimicrobials remains critical to addressing antibiotic resistance and reducing global incidence. Regular screening, prompt treatment, and partner notification are paramount to curbing transmission.