Acute intestinal amebiasis is a parasitic infection caused by Entamoeba histolytica, a protozoan that primarily targets the large intestine. This condition manifests as severe diarrhea, abdominal pain, and, in advanced cases, systemic complications. Globally, it affects approximately 50 million individuals annually, with higher prevalence in regions lacking sanitation infrastructure.
Causes and Transmission Pathways
Entamoeba histolytica spreads via the fecal-oral route, often through contaminated water, food, or direct contact with infected individuals. The parasite exists in two forms: invasive trophozoites and environmentally resistant cysts. Cysts survive outside the host, enabling transmission in unsanitary conditions. Risk factors include poor hygiene, immunosuppression, and travel to endemic areas.
Clinical Symptoms of Amebic Dysentery
Symptom severity ranges from asymptomatic carriage to life-threatening colitis. Common presentations include:
- Watery or bloody diarrhea (amebic dysentery)
- Cramping abdominal pain
- Tenesmus (rectal pain during defecation)
- Fatigue and unintended weight loss
Systemic invasion may lead to hepatic abscesses, pleural effusion, or encephalitis in rare cases.
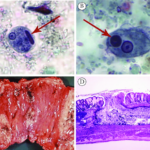
Diagnostic Criteria and Laboratory Testing
Accurate diagnosis relies on stool microscopy, antigen detection, and molecular assays:
- Stool Examination: Identifies cysts or trophozoites in fresh samples.
- Serologic Tests: Detect anti-E. histolytica antibodies (e.g., ELISA).
- PCR: Confirms species-specific DNA in stool or tissue.
Colonoscopy with biopsy is recommended for differentiating amebic ulcers from inflammatory bowel disease.
Evidence-Based Treatment Protocols
First-line therapy combines luminal and tissue-acting agents:
- Metronidazole (500–750 mg TID for 7–10 days): Eradicates invasive trophozoites.
- Paromomycin or Diloxanide Furoate: Eliminate intestinal cysts post-metronidazole.
Severe cases may require intravenous fluids, electrolyte correction, or surgical intervention for perforations.
Complications and Long-Term Prognosis
Untreated amebiasis can progress to toxic megacolon, intestinal perforation, or disseminated infection. Hepatic abscesses present with right upper quadrant pain and fever. Early diagnosis reduces mortality rates to <1%, while delayed treatment increases risks of chronic morbidity.
Prevention and Public Health Strategies
Preventive measures focus on interrupting transmission:
- Boiling or filtering water in endemic regions.
- Hand hygiene with soap after defecation.
- Avoiding raw vegetables or unpeeled fruits in high-risk areas.
Vaccine development remains experimental, emphasizing the need for community education and sanitation improvements.
Acute intestinal amebiasis demands prompt recognition and targeted therapy to prevent complications. Clinicians must prioritize differential diagnosis in high-risk populations and advocate for preventive public health policies. Through interdisciplinary collaboration, morbidity and mortality associated with E. histolytica can be significantly reduced.