Acute hepatic porphyria (AHP) is a group of rare genetic disorders characterized by the accumulation of porphyrins and their precursors in the liver, leading to severe and potentially life-threatening symptoms. This article delves into the intricacies of AHP, providing a detailed overview of its symptoms, causes, diagnostic methods, and treatment options. By understanding the complexities of this condition, patients and healthcare providers can better manage its impact on quality of life.
Acute hepatic porphyria encompasses several disorders, including acute intermittent porphyria (AIP), hereditary coproporphyria (HCP), and variegate porphyria (VP). These conditions arise from genetic mutations that disrupt the heme biosynthesis pathway, specifically in the liver. Heme is a critical component of hemoglobin, and its impaired production leads to the accumulation of toxic porphyrin precursors, causing acute neurovisceral attacks.
Symptoms
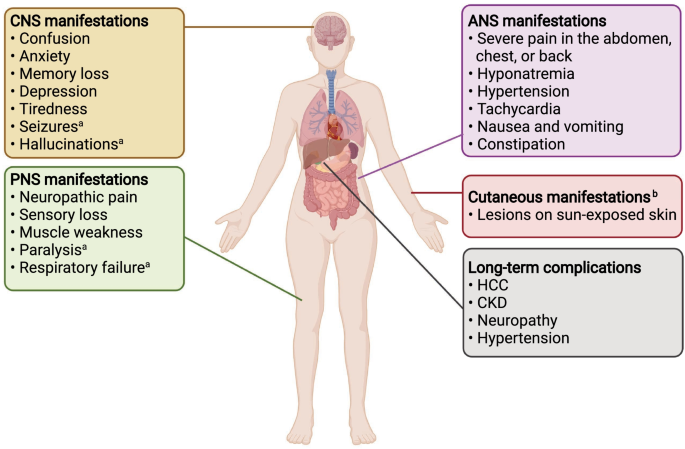
The symptoms of AHP are often nonspecific and can mimic other conditions, making diagnosis challenging. Common symptoms include:
- Severe abdominal pain: Often the most prominent symptom, lasting for days.
- Neurological manifestations: Muscle weakness, seizures, and peripheral neuropathy.
- Psychiatric symptoms: Anxiety, depression, and confusion.
- Gastrointestinal disturbances: Nausea, vomiting, and constipation.
- Cardiovascular issues: Hypertension and tachycardia.
These symptoms are typically episodic, triggered by factors such as hormonal changes, medications, fasting, or infections.
Causes and Genetic Basis
AHP is caused by mutations in genes involved in the heme biosynthesis pathway. The primary genes affected include:
- HMBS: Mutations cause acute intermittent porphyria (AIP).
- CPOX: Mutations lead to hereditary coproporphyria (HCP).
- PPOX: Mutations result in variegate porphyria (VP).
These mutations are inherited in an autosomal dominant pattern, meaning only one copy of the mutated gene is necessary to cause the disorder. However, not all carriers of the mutation experience symptoms, indicating the role of environmental and hormonal triggers.
Diagnosing
Accurate diagnosis of AHP requires a combination of clinical evaluation, biochemical testing, and genetic analysis. Key diagnostic steps include:
- Biochemical Testing: Measurement of porphyrin precursors (ALA and PBG) in urine during an acute attack.
- Genetic Testing: Identification of pathogenic mutations in the relevant genes.
- Differential Diagnosis: Ruling out other conditions with similar symptoms, such as lead poisoning or Guillain-Barré syndrome.
Early diagnosis is crucial to prevent complications and initiate appropriate treatment.
Treatment Options for Acute Hepatic Porphyria
The management of AHP focuses on preventing acute attacks, alleviating symptoms, and addressing long-term complications. Treatment strategies include:
- Acute Attack Management:
- Hematin Infusion: Reduces the production of porphyrin precursors.
- Glucose Administration: Suppresses ALA synthase activity.
- Symptomatic Relief: Pain management with opioids and anti-nausea medications.
- Preventive Measures:
- Avoiding Triggers: Identifying and avoiding medications, fasting, and other triggers.
- Givosiran: An RNAi therapy that reduces ALA synthase levels, approved for recurrent attacks.
- Long-Term Monitoring:
- Regular follow-ups to monitor liver function, renal health, and neurological status.
Living with Acute Hepatic Porphyria
Patients with AHP require a multidisciplinary approach to care, involving hepatologists, neurologists, and genetic counselors. Lifestyle modifications, such as maintaining a balanced diet and avoiding known triggers, are essential. Support groups and patient education can also play a vital role in improving outcomes.
Acute hepatic porphyria is a complex and often misunderstood condition that requires timely diagnosis and comprehensive management. By staying informed about the latest advancements in treatment and adhering to preventive measures, patients can significantly improve their quality of life. This guide serves as a valuable resource for understanding and managing AHP effectively.