Acute gonococcal endometritis is an inflammatory infection of the endometrium caused by Neisseria gonorrhoeae. It is a serious condition that may lead to severe reproductive health complications, including infertility and chronic pelvic pain. Understanding its etiology, risk factors, clinical manifestations, and treatment options is crucial for effective management and prevention.
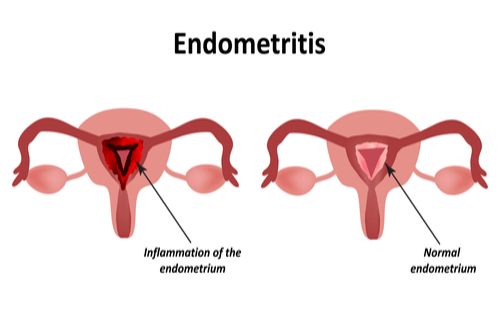
Pathophysiology of Neisseria gonorrhoeae in Endometrial Infection
Neisseria gonorrhoeae is a Gram-negative diplococcus that invades the cervical and endometrial epithelium, triggering an intense inflammatory response. This bacterium produces virulence factors such as:
- Pili and outer membrane proteins that enhance adhesion to epithelial cells.
- Lipooligosaccharides (LOS) that contribute to immune evasion and tissue damage.
- IgA protease, which degrades host antibodies, facilitating bacterial persistence.
Risk Factors for Acute Gonococcal Endometritis
Several factors predispose individuals to N. gonorrhoeae infection and its progression to acute endometritis:
- Unprotected Sexual Activity: High-risk behavior increases transmission.
- Multiple Sexual Partners: Raises exposure to gonorrheal infection.
- History of Sexually Transmitted Infections (STIs): Prior infections heighten susceptibility.
- Compromised Immunity: Conditions such as HIV increase vulnerability.
- Intrauterine Device (IUD) Use: In rare cases, IUDs may facilitate bacterial ascent into the uterus.
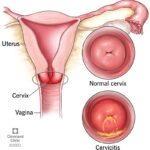
Clinical Symptoms and Diagnosis
Primary Symptoms
- Pelvic Pain: Often severe and persistent.
- Abnormal Vaginal Discharge: Purulent or mucopurulent in nature.
- Intermenstrual Bleeding: Irregular bleeding or spotting.
- Dysuria: Painful urination due to urethral involvement.
- Fever and Malaise: Indicate systemic infection.
Diagnostic Methods for Acute gonococcal endometritis
- Pelvic Examination: Identifies cervical motion tenderness and abnormal discharge.
- Endometrial Biopsy: Confirms inflammation and bacterial presence.
- NAAT (Nucleic Acid Amplification Test): Detects N. gonorrhoeae DNA.
- Gram Stain and Culture: Identifies Gram-negative intracellular diplococci.
- Ultrasound or MRI: Helps rule out abscess formation or other pelvic pathologies.
Treatment Strategies for Acute gonococcal endometritis
1. Antibiotic Therapy
- Ceftriaxone (500 mg IM single dose) combined with Doxycycline (100 mg twice daily for 14 days).
- Alternative Regimens: Azithromycin (if doxycycline is contraindicated).
- Empirical Treatment: In co-infections with Chlamydia trachomatis.
2. Supportive Care
- Pain Management: NSAIDs like ibuprofen help alleviate pelvic pain.
- Hydration and Rest: Essential for recovery and symptom relief.
3. Partner Notification and Treatment
- Expedited Partner Therapy (EPT): Prevents reinfection and transmission.
- Screening and Counseling: Educate patients on STI prevention.
Potential Complications
If left untreated, acute gonococcal endometritis can lead to:
- Pelvic Inflammatory Disease (PID): A major cause of infertility.
- Tubal Factor Infertility: Due to fallopian tube scarring.
- Ectopic Pregnancy: Increased risk due to tubal damage.
- Chronic Pelvic Pain: Resulting from persistent inflammation.
- Septicemia: Rare but life-threatening systemic infection.
Prevention and Public Health Strategies
- Consistent Condom Use: Reduces transmission risk.
- Regular STI Screening: Especially for sexually active individuals.
- Timely Treatment of STIs: Prevents progression to complications.
- HPV and STI Education: Enhances awareness and risk reduction.
Acute gonococcal endometritis is a severe infection requiring prompt diagnosis and treatment. Effective antibiotic regimens, preventive measures, and patient education are critical in reducing morbidity and preventing long-term complications. Regular screening and safe sexual practices remain the cornerstone of prevention.