Clostridium tubo-ovarian abscess (TOA) is a severe and often life-threatening infection that involves the female reproductive organs, particularly the ovaries and fallopian tubes. This infection, commonly caused by Clostridium species, leads to the formation of abscesses and can result in systemic sepsis if left untreated. While tubo-ovarian abscesses are typically associated with other bacterial infections, the involvement of Clostridium species adds an additional layer of complexity due to their anaerobic nature and ability to cause rapid tissue necrosis.
In this article, we explore the causes, symptoms, diagnostic methods, and treatment options for Clostridium tubo-ovarian abscess, providing healthcare professionals and patients with a thorough understanding of this dangerous infection.
What Is Clostridium Tubo-Ovarian Abscess?
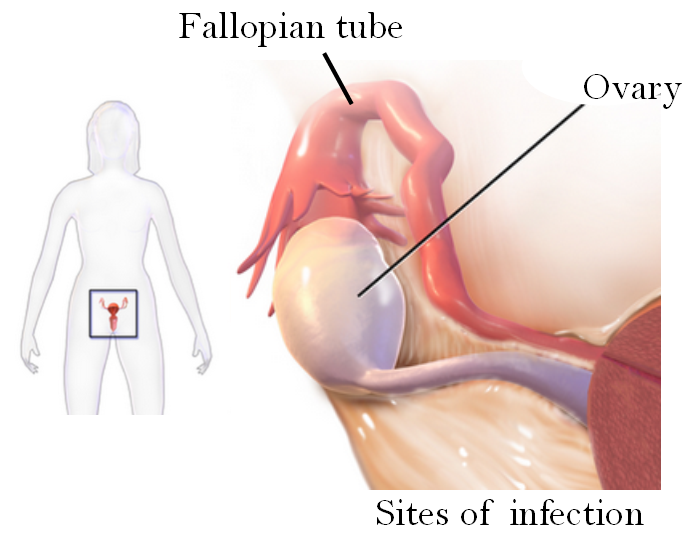
A tubo-ovarian abscess (TOA) occurs when an infection in the reproductive tract causes pus to accumulate within the ovaries or fallopian tubes. Clostridium species, primarily anaerobic bacteria, can cause these abscesses, leading to inflammation, pain, and tissue destruction. Clostridium species, including Clostridium perfringens, Clostridium septicum, and Clostridium sordellii, are capable of producing potent toxins that exacerbate the infection, resulting in severe symptoms and potential complications such as septic shock.
Pathophysiology of Clostridium Tubo-Ovarian Abscess
Clostridium bacteria are typically introduced into the pelvic cavity through conditions such as pelvic inflammatory disease (PID), post-abortion infections, or after a surgical procedure. Once the bacteria enter the reproductive organs, they proliferate and produce toxins that lead to tissue necrosis, abscess formation, and systemic infection. Due to their anaerobic nature, Clostridium species thrive in environments with low oxygen levels, making the ovaries and fallopian tubes an ideal site for infection.
Symptoms of Clostridium Tubo-Ovarian Abscess
Clostridium tubo-ovarian abscess manifests with a range of clinical symptoms. While the severity of symptoms may vary, the following are commonly observed in patients:
- Pelvic Pain: A hallmark symptom of TOA, often described as severe, localized, and sharp.
- Abdominal Distension: In cases where the abscesses have grown significantly, the abdomen may become swollen or tender to touch.
- Fever and Chills: A high fever, accompanied by chills, may indicate the progression of sepsis.
- Vaginal Discharge: Abnormal discharge, sometimes foul-smelling, may occur as a result of the infection.
- Nausea and Vomiting: These gastrointestinal symptoms can occur due to the systemic effects of the infection.
- Dyspareunia: Pain during intercourse is another common symptom in women with TOA.
The progression of the infection can lead to serious complications, including septic shock and organ failure, if not addressed promptly.
Causes of Clostridium Tubo-Ovarian Abscess
Clostridium tubo-ovarian abscess is primarily caused by an infection with anaerobic bacteria from the Clostridium genus. Several factors contribute to the development of this infection:
- Pelvic Inflammatory Disease (PID): This is the most common precursor to TOA. PID is an infection of the female reproductive organs, often caused by sexually transmitted infections (STIs) like Chlamydia or Gonorrhea, which can increase the risk of a TOA.
- Post-Surgical or Post-Abortion Infections: Invasive procedures, including surgeries or abortions, can introduce Clostridium bacteria into the reproductive organs, leading to infection.
- Tissue Necrosis and Ischemia: The low oxygen environment in damaged tissues provides an ideal setting for anaerobic bacteria, including Clostridium, to proliferate.
- Compromised Immune System: Individuals with weakened immune defenses are at an increased risk of developing severe infections, including Clostridium TOA.
Diagnosis
Diagnosis of Clostridium tubo-ovarian abscess involves a combination of clinical evaluation and imaging studies. The following steps are essential in diagnosing this condition:
1. Clinical Evaluation
Healthcare providers typically assess the patient’s medical history, symptoms, and risk factors. A thorough pelvic examination is critical to identify tenderness, swelling, or signs of an abscess. Additionally, any history of pelvic inflammatory disease, recent surgeries, or abortion should be noted.
2. Imaging Studies
- Transvaginal Ultrasound: This is the most commonly used imaging modality to detect tubo-ovarian abscesses. It can reveal the presence of fluid-filled masses in the pelvic cavity, which may indicate an abscess.
- CT Scan or MRI: In complicated cases, a CT scan or MRI may provide more detailed information about the size, location, and extent of the abscess.
- X-ray: If gas is present in the abscess, an X-ray may show air bubbles, which is a hallmark sign of a Clostridium infection.
3. Microbiological Culture
To confirm the presence of Clostridium species, a sample of the abscess fluid or vaginal discharge may be collected and cultured. This helps identify the specific Clostridium species responsible for the infection and determine antibiotic sensitivity.
Treatment of Clostridium Tubo-Ovarian Abscess
The treatment of Clostridium tubo-ovarian abscess involves both medical management and, in some cases, surgical intervention. The goal of treatment is to control the infection, manage complications, and preserve fertility when possible.
1. Antibiotic Therapy
Due to the anaerobic nature of Clostridium species, broad-spectrum intravenous (IV) antibiotics are typically administered as the first line of treatment. The choice of antibiotics may include:
- Clindamycin
- Metronidazole
- Ampicillin/Sulbactam
- Piperacillin/Tazobactam
Once the specific Clostridium species is identified through culture, antibiotic therapy may be adjusted accordingly.
2. Surgical Drainage
If the abscess is large or if the patient is experiencing severe symptoms such as sepsis, surgical drainage may be necessary. This procedure involves draining the pus from the abscess to alleviate pressure and reduce the risk of further complications.
3. Supportive Care
In severe cases, supportive care is essential to manage sepsis and prevent organ failure. This may involve fluid resuscitation, oxygen therapy, and vasopressor medications to stabilize blood pressure.
Potential Complications of Clostridium Tubo-Ovarian Abscess
Failure to treat Clostridium tubo-ovarian abscess promptly can result in severe complications, including:
- Septic Shock: A life-threatening condition that occurs when the infection spreads throughout the body, leading to systemic inflammation and organ failure.
- Peritonitis: Inflammation of the peritoneum, the lining of the abdominal cavity, which can result from the rupture of the abscess.
- Infertility: In some cases, the infection can damage the ovaries or fallopian tubes, leading to permanent infertility.
- Toxic Shock Syndrome (TSS): Caused by the release of toxins from the Clostridium bacteria, this syndrome can lead to multi-organ failure.
Prevention of Clostridium Tubo-Ovarian Abscess
Preventing Clostridium tubo-ovarian abscess requires addressing the underlying risk factors. Some preventive measures include:
- Timely Treatment of Pelvic Inflammatory Disease (PID): Early intervention with antibiotics can reduce the risk of developing TOA.
- Safe Surgical Practices: Proper sterilization and techniques during surgeries and abortions can minimize the risk of introducing Clostridium bacteria into the reproductive tract.
- Safe Sexual Practices: Practicing safe sex and getting regular screenings for STIs can help prevent PID and its complications.