Clostridium peritonitis is a severe and potentially fatal bacterial infection that primarily affects the abdominal cavity. It is caused by the bacteria Clostridium, often Clostridium perfringens, which can rapidly multiply in the abdominal environment, leading to a series of dangerous health complications. This article delves into the key aspects of Clostridium peritonitis, including its causes, symptoms, diagnostic methods, treatment options, and preventive measures.
What is Clostridium Peritonitis?
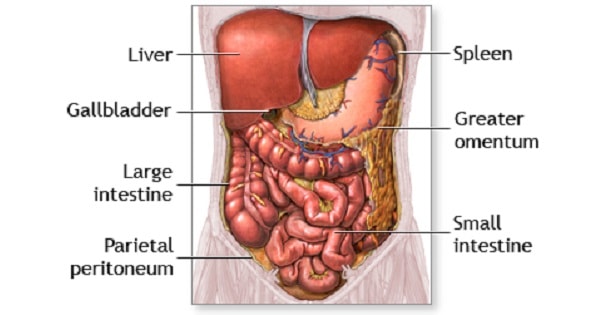
Clostridium peritonitis refers to an infection of the peritoneum, the lining that covers the abdominal organs, caused by the Clostridium species of bacteria. The condition typically results from a breach in the abdominal wall or digestive tract, allowing the bacteria to enter the sterile abdominal cavity. While Clostridium perfringens is the most common strain involved, other species such as Clostridium difficile and Clostridium septicum can also be implicated in some cases.
The Role of Clostridium Bacteria
Clostridium is a genus of bacteria that thrives in environments lacking oxygen. This makes the abdominal cavity an ideal setting for their growth, particularly after surgeries, traumatic injuries, or infections that compromise the digestive system’s integrity. The bacteria can cause gas gangrene, a serious condition where tissues die due to bacterial infection, leading to systemic symptoms such as fever, tachycardia, and severe abdominal pain.
Causes of Clostridium Peritonitis
The main cause of Clostridium peritonitis is the introduction of Clostridium bacteria into the peritoneal cavity. Several factors can contribute to the onset of this infection:
- Traumatic Injury or Surgery: Abdominal trauma, such as a gunshot or stabbing wound, or abdominal surgeries like appendectomy or colon resection, can expose the abdominal cavity to these bacteria.
- Perforation of the Gastrointestinal Tract: Conditions such as diverticulitis, Crohn’s disease, or peptic ulcers can lead to perforations in the intestines, allowing Clostridium bacteria to enter the peritoneum.
- Intra-abdominal Abscesses: Pre-existing abscesses in the abdomen caused by other infections can serve as a breeding ground for Clostridium bacteria, increasing the risk of peritonitis.
- Immune System Compromise: Individuals with weakened immune systems, such as those with diabetes, cancer, or liver disease, are more susceptible to Clostridium infections.
Symptoms of Clostridium Peritonitis
The clinical presentation of Clostridium peritonitis varies depending on the severity of the infection, but common symptoms include:
Initial Symptoms:
- Severe Abdominal Pain: Typically localized to the affected area, this pain may be sudden and intense.
- Swelling or Distension: The abdomen may become visibly swollen as the infection progresses.
- Fever and Chills: A hallmark of most infections, fever and chills signal the body’s immune response to the invading bacteria.
Progressive Symptoms:
- Sepsis: If left untreated, the infection can lead to sepsis, marked by rapid heart rate, low blood pressure, confusion, and organ failure.
- Tachycardia: An increased heart rate is commonly seen in cases of severe infection.
- Nausea and Vomiting: These symptoms are often associated with the body’s attempt to fight the infection.
The presence of gas under the skin, a condition known as crepitus, can also occur in cases of Clostridium peritonitis due to the production of gas by the bacteria.
Diagnosis of Clostridium Peritonitis
Timely diagnosis is crucial in managing Clostridium peritonitis effectively. Healthcare providers rely on a combination of clinical examination, imaging, and laboratory tests to confirm the presence of the infection.
Clinical Examination:
Upon physical examination, a healthcare provider may find signs of peritoneal irritation, such as tenderness, guarding, and rebound tenderness. Abdominal distention may also be observed.
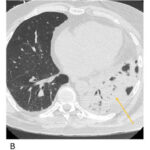
Imaging Techniques:
- Abdominal X-ray: Can show signs of perforation, gas in the peritoneal cavity, or bowel obstruction.
- CT Scan: This is the gold standard for identifying perforations, abscesses, and the extent of infection in the abdominal cavity. It can also help detect gas bubbles under the skin or within the peritoneal cavity.
- Ultrasound: Useful for detecting fluid collections or abscesses in the abdomen.
Laboratory Tests:
- Blood Cultures: These tests are crucial for identifying the specific strain of Clostridium responsible for the infection.
- Peritoneal Fluid Analysis: Fluid obtained from the peritoneal cavity during diagnostic laparoscopy can be analyzed for the presence of bacteria.
Treatment of Clostridium Peritonitis
The treatment of Clostridium peritonitis is multifaceted and often requires a combination of surgical intervention and aggressive antibiotic therapy.
Surgical Intervention:
Surgical management is often necessary to remove the source of infection. This may involve:
- Drainage of Abscesses: Abscesses filled with pus or infected fluid need to be drained to reduce the bacterial load.
- Repair of Perforations: If an organ such as the intestine is perforated, surgical repair is essential to close the breach and prevent further contamination.
- Debridement of Infected Tissue: In severe cases, removal of necrotic tissue is necessary to prevent the infection from spreading.
Antibiotic Therapy:
Broad-spectrum intravenous antibiotics are administered to control the bacterial infection. Commonly used antibiotics include:
- Penicillins (e.g., Penicillin G)
- Clindamycin
- Metronidazole
- Carbapenems (e.g., Meropenem)
Once the specific strain of Clostridium is identified, antibiotic therapy may be adjusted to target the bacteria more effectively.
Supportive Care:
Patients with severe Clostridium peritonitis may require intensive care to manage sepsis, fluid imbalances, and organ dysfunction. This may include intravenous fluids, vasopressors to support blood pressure, and mechanical ventilation if necessary.
Prevention of Clostridium Peritonitis
Prevention of Clostridium peritonitis revolves around minimizing the risk of bacterial entry into the peritoneal cavity. Key preventive measures include:
- Proper Wound Care: Ensuring proper sterilization and cleaning of any abdominal wounds or surgical sites can reduce the risk of infection.
- Timely Treatment of Gastrointestinal Conditions: Early intervention for conditions like diverticulitis, Crohn’s disease, or peptic ulcers can prevent perforations.
- Use of Prophylactic Antibiotics: In patients undergoing abdominal surgery, prophylactic antibiotics may be prescribed to reduce the risk of infection.
Additionally, individuals with compromised immune systems should take extra precautions, including close monitoring for any signs of infection following abdominal procedures or trauma.
Prognosis and Outlook
The prognosis for Clostridium peritonitis depends on several factors, including the timeliness of diagnosis, the severity of the infection, and the patient’s overall health. With appropriate and timely treatment, many patients recover fully, though the condition can be fatal if left untreated. Prompt surgical intervention and targeted antibiotic therapy are critical to improving outcomes.