Clostridium perfringens empyema, a Gram-positive, spore-forming anaerobic bacterium, is predominantly recognized for its role in gas gangrene and food poisoning. However, its involvement in pleuropulmonary infections, particularly empyema, remains relatively rare but clinically significant. Empyema refers to the accumulation of pus within the pleural cavity, and when caused by C. perfringens, it presents unique diagnostic and therapeutic challenges.
Pathogenesis
The development of C. perfringens empyema is often associated with specific predisposing factors:
- Trauma or Invasive Procedures: Penetrating chest injuries or surgical interventions can introduce the bacterium into the pleural space.
- Aspiration: Inhalation of oropharyngeal contents, especially in individuals with swallowing dysfunction, can lead to infection.
- Hematogenous Spread: Bacteremic dissemination from distant infection sites may seed the pleura.
Notably, cases have been documented where C. perfringens empyema developed without any identifiable risk factors, underscoring the bacterium’s opportunistic potential.
Clinical Manifestations
Patients with C. perfringens empyema may exhibit a range of symptoms:
- Respiratory Symptoms: Shortness of breath, cough (often nonproductive), and pleuritic chest pain.
- Systemic Signs: Fever, chills, and general malaise.
- Physical Examination: Decreased breath sounds and dullness to percussion over the affected area.
In some instances, the presentation may be insidious, with mild symptoms despite significant pleural involvement.
Diagnostic Approaches
Accurate diagnosis involves a combination of clinical evaluation and diagnostic testing:
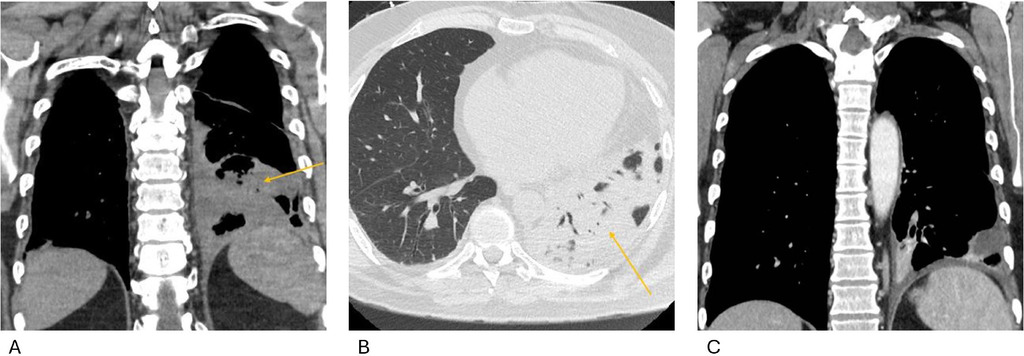
- Imaging Studies: Chest radiographs and computed tomography (CT) scans can reveal pleural effusion, gas within the pleural space, and associated lung parenchymal changes.
- Thoracentesis: Aspiration of pleural fluid allows for analysis, typically revealing:
- Appearance: Foul-smelling, dark-colored fluid.
- Laboratory Findings: Low pH, elevated lactate dehydrogenase (LDH), and high protein content.
- Microbiological Studies: Gram stain and culture of pleural fluid are essential to identify C. perfringens and determine antibiotic susceptibility.
Early recognition is crucial, as delayed diagnosis can lead to complications such as necrotizing pneumonia and septic shock.
Treatment Strategies
Management of C. perfringens empyema requires a multifaceted approach:
- Antibiotic Therapy: Empirical broad-spectrum antibiotics should be initiated promptly, later tailored based on culture results. Penicillin remains the drug of choice, often combined with agents like clindamycin to inhibit toxin production.
- Source Control: Effective drainage of the pleural space is vital. Options include:
- Chest Tube Placement: Facilitates continuous drainage of infected fluid.
- Intrapleural Fibrinolytics: Agents such as tissue plasminogen activator (tPA) and DNase may be used to enhance drainage, especially in cases with loculated effusions.
- Surgical Intervention: Procedures like decortication may be necessary for patients with organized empyema or when less invasive measures fail.
- Supportive Care: Includes oxygen therapy, analgesia, and management of comorbid conditions.
Early and aggressive treatment is associated with favorable outcomes, whereas delays can result in increased morbidity and mortality.